User login
-
Few Cancer Survivors Meet ACS Nutrition, Exercise Guidelines
TOPLINE:
METHODOLOGY:
- The ACS has published nutrition and exercise guidelines for cancer survivors, which include recommendations to maintain a healthy weight and diet, cut out alcohol, and participate in regular physical activities. Engaging in these behaviors is associated with longer survival among cancer survivors, but whether survivors follow these nutrition and activity recommendations has not been systematically tracked.
- Researchers evaluated data on 10,020 individuals (mean age, 64.2 years) who had completed cancer treatment. Data came from the Behavioral Risk Factor Surveillance System telephone-based survey administered in 2017, 2019, and 2021, which represents 2.7 million cancer survivors.
- The researchers estimated survivors’ adherence to guidelines across four domains: Weight, physical activity, fruit and vegetable consumption, and alcohol intake. Factors associated with adherence were also evaluated.
- Overall, 9,121 survivors (91%) completed questionnaires for all four domains.
TAKEAWAY:
Only 4% of patients (365 of 9121) followed ACS guidelines in all four categories.
When assessing adherence to each category, the researchers found that 72% of cancer survivors reported engaging in recommended levels of physical activity, 68% maintained a nonobese weight, 50% said they did not consume alcohol, and 12% said they consumed recommended quantities of fruits and vegetables.
Compared with people in the general population, cancer survivors generally engaged in fewer healthy behaviors than those who had never been diagnosed with cancer.
The authors identified certain factors associated with greater guideline adherence, including female sex, older age, Black (vs White) race, and higher education level (college graduate).
IN PRACTICE:
This study highlights a potential “gap between published guidelines regarding behavioral modifications for cancer survivors and uptake of these behaviors,” the authors wrote, adding that “it is essential for oncologists and general internists to improve widespread and systematic counseling on these guidelines to improve uptake of healthy behaviors in this vulnerable patient population.”
SOURCE:
This work, led by Carter Baughman, MD, from the Division of Internal Medicine at Beth Israel Deaconess Medical Center, Boston, Massachusetts, was published online in JAMA Oncology.
LIMITATIONS:
The authors reported several study limitations, most notably that self-reported data may introduce biases.
DISCLOSURES:
The study funding source was not reported. One author received grants from the US Highbush Blueberry Council outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The ACS has published nutrition and exercise guidelines for cancer survivors, which include recommendations to maintain a healthy weight and diet, cut out alcohol, and participate in regular physical activities. Engaging in these behaviors is associated with longer survival among cancer survivors, but whether survivors follow these nutrition and activity recommendations has not been systematically tracked.
- Researchers evaluated data on 10,020 individuals (mean age, 64.2 years) who had completed cancer treatment. Data came from the Behavioral Risk Factor Surveillance System telephone-based survey administered in 2017, 2019, and 2021, which represents 2.7 million cancer survivors.
- The researchers estimated survivors’ adherence to guidelines across four domains: Weight, physical activity, fruit and vegetable consumption, and alcohol intake. Factors associated with adherence were also evaluated.
- Overall, 9,121 survivors (91%) completed questionnaires for all four domains.
TAKEAWAY:
Only 4% of patients (365 of 9121) followed ACS guidelines in all four categories.
When assessing adherence to each category, the researchers found that 72% of cancer survivors reported engaging in recommended levels of physical activity, 68% maintained a nonobese weight, 50% said they did not consume alcohol, and 12% said they consumed recommended quantities of fruits and vegetables.
Compared with people in the general population, cancer survivors generally engaged in fewer healthy behaviors than those who had never been diagnosed with cancer.
The authors identified certain factors associated with greater guideline adherence, including female sex, older age, Black (vs White) race, and higher education level (college graduate).
IN PRACTICE:
This study highlights a potential “gap between published guidelines regarding behavioral modifications for cancer survivors and uptake of these behaviors,” the authors wrote, adding that “it is essential for oncologists and general internists to improve widespread and systematic counseling on these guidelines to improve uptake of healthy behaviors in this vulnerable patient population.”
SOURCE:
This work, led by Carter Baughman, MD, from the Division of Internal Medicine at Beth Israel Deaconess Medical Center, Boston, Massachusetts, was published online in JAMA Oncology.
LIMITATIONS:
The authors reported several study limitations, most notably that self-reported data may introduce biases.
DISCLOSURES:
The study funding source was not reported. One author received grants from the US Highbush Blueberry Council outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- The ACS has published nutrition and exercise guidelines for cancer survivors, which include recommendations to maintain a healthy weight and diet, cut out alcohol, and participate in regular physical activities. Engaging in these behaviors is associated with longer survival among cancer survivors, but whether survivors follow these nutrition and activity recommendations has not been systematically tracked.
- Researchers evaluated data on 10,020 individuals (mean age, 64.2 years) who had completed cancer treatment. Data came from the Behavioral Risk Factor Surveillance System telephone-based survey administered in 2017, 2019, and 2021, which represents 2.7 million cancer survivors.
- The researchers estimated survivors’ adherence to guidelines across four domains: Weight, physical activity, fruit and vegetable consumption, and alcohol intake. Factors associated with adherence were also evaluated.
- Overall, 9,121 survivors (91%) completed questionnaires for all four domains.
TAKEAWAY:
Only 4% of patients (365 of 9121) followed ACS guidelines in all four categories.
When assessing adherence to each category, the researchers found that 72% of cancer survivors reported engaging in recommended levels of physical activity, 68% maintained a nonobese weight, 50% said they did not consume alcohol, and 12% said they consumed recommended quantities of fruits and vegetables.
Compared with people in the general population, cancer survivors generally engaged in fewer healthy behaviors than those who had never been diagnosed with cancer.
The authors identified certain factors associated with greater guideline adherence, including female sex, older age, Black (vs White) race, and higher education level (college graduate).
IN PRACTICE:
This study highlights a potential “gap between published guidelines regarding behavioral modifications for cancer survivors and uptake of these behaviors,” the authors wrote, adding that “it is essential for oncologists and general internists to improve widespread and systematic counseling on these guidelines to improve uptake of healthy behaviors in this vulnerable patient population.”
SOURCE:
This work, led by Carter Baughman, MD, from the Division of Internal Medicine at Beth Israel Deaconess Medical Center, Boston, Massachusetts, was published online in JAMA Oncology.
LIMITATIONS:
The authors reported several study limitations, most notably that self-reported data may introduce biases.
DISCLOSURES:
The study funding source was not reported. One author received grants from the US Highbush Blueberry Council outside the submitted work. No other disclosures were reported.
A version of this article appeared on Medscape.com.
<!--$RCSfile: InCopy_agile.xsl,v $ $Revision: 1.35 $-->
<!--$RCSfile: drupal.xsl,v $ $Revision: 1.7 $-->
<root generator="drupal.xsl" gversion="1.7"> <header> <fileName>167860</fileName> <TBEID>0C04FD2C.SIG</TBEID> <TBUniqueIdentifier>MD_0C04FD2C</TBUniqueIdentifier> <newsOrJournal>News</newsOrJournal> <publisherName>Frontline Medical Communications</publisherName> <storyname/> <articleType>2</articleType> <TBLocation>QC Done-All Pubs</TBLocation> <QCDate>20240426T151917</QCDate> <firstPublished>20240426T152032</firstPublished> <LastPublished>20240426T152032</LastPublished> <pubStatus qcode="stat:"/> <embargoDate/> <killDate/> <CMSDate>20240426T152032</CMSDate> <articleSource/> <facebookInfo/> <meetingNumber/> <byline>Deepa Varma</byline> <bylineText>DEEPA VARMA</bylineText> <bylineFull>DEEPA VARMA</bylineFull> <bylineTitleText/> <USOrGlobal/> <wireDocType/> <newsDocType>News</newsDocType> <journalDocType/> <linkLabel/> <pageRange/> <citation/> <quizID/> <indexIssueDate/> <itemClass qcode="ninat:text"/> <provider qcode="provider:imng"> <name>IMNG Medical Media</name> <rightsInfo> <copyrightHolder> <name>Frontline Medical News</name> </copyrightHolder> <copyrightNotice>Copyright (c) 2015 Frontline Medical News, a Frontline Medical Communications Inc. company. All rights reserved. This material may not be published, broadcast, copied, or otherwise reproduced or distributed without the prior written permission of Frontline Medical Communications Inc.</copyrightNotice> </rightsInfo> </provider> <abstract/> <metaDescription>A recent survey-based study found that only 4% of cancer survivors reported adhering to all four American Cancer Society (ACS) nutrition and physical activity g</metaDescription> <articlePDF/> <teaserImage/> <teaser>Researchers estimate more than 9,000 survivors’ adherence to weight, physical activity, fruit and vegetable consumption, and alcohol intake guidelines.</teaser> <title>Few Cancer Survivors Meet ACS Nutrition, Exercise Guidelines</title> <deck/> <disclaimer/> <AuthorList/> <articleURL/> <doi/> <pubMedID/> <publishXMLStatus/> <publishXMLVersion>1</publishXMLVersion> <useEISSN>0</useEISSN> <urgency/> <pubPubdateYear/> <pubPubdateMonth/> <pubPubdateDay/> <pubVolume/> <pubNumber/> <wireChannels/> <primaryCMSID/> <CMSIDs/> <keywords/> <seeAlsos/> <publications_g> <publicationData> <publicationCode>oncr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>hemn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>chph</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>fp</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>im</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>ob</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>nr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle>Neurology Reviews</journalTitle> <journalFullTitle>Neurology Reviews</journalFullTitle> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>skin</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>GIHOLD</publicationCode> <pubIssueName>January 2014</pubIssueName> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement/> </publicationData> </publications_g> <publications> <term canonical="true">31</term> <term>18</term> <term>6</term> <term>15</term> <term>21</term> <term>23</term> <term>22</term> <term>13</term> </publications> <sections> <term canonical="true">27970</term> <term>39313</term> <term>86</term> </sections> <topics> <term>270</term> <term canonical="true">280</term> <term>198</term> <term>61821</term> <term>59244</term> <term>67020</term> <term>214</term> <term>217</term> <term>221</term> <term>238</term> <term>240</term> <term>242</term> <term>244</term> <term>39570</term> <term>245</term> <term>31848</term> <term>292</term> <term>178</term> <term>179</term> <term>181</term> <term>59374</term> <term>196</term> <term>197</term> <term>37637</term> <term>233</term> <term>243</term> <term>250</term> <term>49434</term> <term>303</term> <term>263</term> <term>192</term> <term>256</term> </topics> <links/> </header> <itemSet> <newsItem> <itemMeta> <itemRole>Main</itemRole> <itemClass>text</itemClass> <title>Few Cancer Survivors Meet ACS Nutrition, Exercise Guidelines</title> <deck/> </itemMeta> <itemContent> <h2>TOPLINE:</h2> <p> <span class="tag metaDescription">A recent survey-based study found that only 4% of cancer survivors reported adhering to all four American Cancer Society (ACS) nutrition and physical activity guidelines, which include maintaining a healthy weight and diet, avoiding alcohol, and exercising regularly.</span> </p> <h2>METHODOLOGY:</h2> <ul class="body"> <li>The ACS has published nutrition and exercise guidelines for cancer survivors, which include recommendations to maintain a healthy weight and diet, cut out alcohol, and participate in regular physical activities. Engaging in these behaviors is associated with longer survival among cancer survivors, but whether survivors follow these nutrition and activity recommendations has not been systematically tracked.</li> <li>Researchers evaluated data on 10,020 individuals (mean age, 64.2 years) who had completed cancer treatment. Data came from the Behavioral Risk Factor Surveillance System telephone-based survey administered in 2017, 2019, and 2021, which represents 2.7 million cancer survivors.</li> <li>The researchers estimated survivors’ adherence to guidelines across four domains: Weight, physical activity, fruit and vegetable consumption, and alcohol intake. Factors associated with adherence were also evaluated.</li> <li>Overall, 9,121 survivors (91%) completed questionnaires for all four domains.</li> </ul> <h2>TAKEAWAY:</h2> <p>Only 4% of patients (365 of 9121) followed ACS guidelines in all four categories.<br/><br/>When assessing adherence to each category, the researchers found that 72% of cancer survivors reported engaging in recommended levels of physical activity, 68% maintained a nonobese weight, 50% said they did not consume alcohol, and 12% said they consumed recommended quantities of fruits and vegetables.<br/><br/>Compared with people in the general population, cancer survivors generally engaged in fewer healthy behaviors than those who had never been diagnosed with cancer.<br/><br/>The authors identified certain factors associated with greater guideline adherence, including female sex, older age, Black (vs White) race, and higher education level (college graduate).</p> <h2>IN PRACTICE:</h2> <p>This study highlights a potential “gap between published guidelines regarding behavioral modifications for cancer survivors and uptake of these behaviors,” the authors wrote, adding that “it is essential for oncologists and general internists to improve widespread and systematic counseling on these guidelines to improve uptake of healthy behaviors in this vulnerable patient population.”</p> <h2>SOURCE:</h2> <p>This work, led by Carter Baughman, MD, from the Division of Internal Medicine at Beth Israel Deaconess Medical Center, Boston, Massachusetts, was published <span class="Hyperlink"><a href="https://jamanetwork.com/journals/jamaoncology/fullarticle/2817661">online</a></span> in <em>JAMA Oncology</em>.</p> <h2>LIMITATIONS:</h2> <p>The authors reported several study limitations, most notably that self-reported data may introduce biases.</p> <h2>DISCLOSURES:</h2> <p>The study funding source was not reported. One author received grants from the US Highbush Blueberry Council outside the submitted work. No other disclosures were reported.<span class="end"/></p> <p> <em>A version of this article appeared on <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/few-cancer-survivors-meet-acs-nutrition-exercise-guidelines-2024a10007sl?src=">Medscape.com</a></span>.</em> </p> </itemContent> </newsItem> <newsItem> <itemMeta> <itemRole>teaser</itemRole> <itemClass>text</itemClass> <title/> <deck/> </itemMeta> <itemContent> </itemContent> </newsItem> </itemSet></root>
FDA Approves Second Gene Therapy for Hemophilia B
Patients are eligible for a one-time infusion of Pfizer’s gene therapy if they are currently using clotting factor IX prophylaxis therapy; have current or historical life-threatening hemorrhages; or have repeated, serious spontaneous bleeding episodes.
Beqvez is the second gene therapy the agency has approved for hemophilia B, a deficiency in clotting factor IX because of a faulty gene that occurs mostly in males. The FDA approved the first gene therapy, etranacogene dezaparvovec (Hemgenix), in November 2022.
Both therapies deliver a functional copy of the factor IX gene to liver cells via a viral vector.
Pfizer said the list price of Beqvez will be $3.5 million — the same price as Hemgenix. The argument for this hefty price tag is that these gene therapies offer the possibility of a cure whereas ongoing factor IX infusions can cost more than $20 million over a patient’s lifetime. Uptake of Hemgenix, however, has been slow, given the cost and concerns about the therapy’s durability and safety.
Beqvez was approved on the basis of the phase 3 BENEGENE-2 trial in 45 men with moderate to severe hemophilia B. These men had been on factor IX prophylaxis for at least 6 months and had tested negative for antibodies against the viral delivery vector.
The annualized bleeding rate fell from a mean of 4.5 events during the pretreatment period of at least 6 months to a mean of 2.5 events between week 12 and data cutoff (median, 1.8 years of follow-up), according to Pfizer’s press release. Overall, bleeding events were eliminated in 60% of patients who received the one-time infusion vs 29% of patients on factor IX prophylaxis therapy.
Overall, Pfizer reported that the gene therapy was “generally well-tolerated,” with an increase in transaminases reported as the most common adverse event. No deaths, serious infusion reactions, thrombotic events, or development of factor IX antibodies occurred.
Pfizer has said it will continue to monitor patients to assess the therapy’s long-term durability and safety over a 15-year period.
A version of this article appeared on Medscape.com.
Patients are eligible for a one-time infusion of Pfizer’s gene therapy if they are currently using clotting factor IX prophylaxis therapy; have current or historical life-threatening hemorrhages; or have repeated, serious spontaneous bleeding episodes.
Beqvez is the second gene therapy the agency has approved for hemophilia B, a deficiency in clotting factor IX because of a faulty gene that occurs mostly in males. The FDA approved the first gene therapy, etranacogene dezaparvovec (Hemgenix), in November 2022.
Both therapies deliver a functional copy of the factor IX gene to liver cells via a viral vector.
Pfizer said the list price of Beqvez will be $3.5 million — the same price as Hemgenix. The argument for this hefty price tag is that these gene therapies offer the possibility of a cure whereas ongoing factor IX infusions can cost more than $20 million over a patient’s lifetime. Uptake of Hemgenix, however, has been slow, given the cost and concerns about the therapy’s durability and safety.
Beqvez was approved on the basis of the phase 3 BENEGENE-2 trial in 45 men with moderate to severe hemophilia B. These men had been on factor IX prophylaxis for at least 6 months and had tested negative for antibodies against the viral delivery vector.
The annualized bleeding rate fell from a mean of 4.5 events during the pretreatment period of at least 6 months to a mean of 2.5 events between week 12 and data cutoff (median, 1.8 years of follow-up), according to Pfizer’s press release. Overall, bleeding events were eliminated in 60% of patients who received the one-time infusion vs 29% of patients on factor IX prophylaxis therapy.
Overall, Pfizer reported that the gene therapy was “generally well-tolerated,” with an increase in transaminases reported as the most common adverse event. No deaths, serious infusion reactions, thrombotic events, or development of factor IX antibodies occurred.
Pfizer has said it will continue to monitor patients to assess the therapy’s long-term durability and safety over a 15-year period.
A version of this article appeared on Medscape.com.
Patients are eligible for a one-time infusion of Pfizer’s gene therapy if they are currently using clotting factor IX prophylaxis therapy; have current or historical life-threatening hemorrhages; or have repeated, serious spontaneous bleeding episodes.
Beqvez is the second gene therapy the agency has approved for hemophilia B, a deficiency in clotting factor IX because of a faulty gene that occurs mostly in males. The FDA approved the first gene therapy, etranacogene dezaparvovec (Hemgenix), in November 2022.
Both therapies deliver a functional copy of the factor IX gene to liver cells via a viral vector.
Pfizer said the list price of Beqvez will be $3.5 million — the same price as Hemgenix. The argument for this hefty price tag is that these gene therapies offer the possibility of a cure whereas ongoing factor IX infusions can cost more than $20 million over a patient’s lifetime. Uptake of Hemgenix, however, has been slow, given the cost and concerns about the therapy’s durability and safety.
Beqvez was approved on the basis of the phase 3 BENEGENE-2 trial in 45 men with moderate to severe hemophilia B. These men had been on factor IX prophylaxis for at least 6 months and had tested negative for antibodies against the viral delivery vector.
The annualized bleeding rate fell from a mean of 4.5 events during the pretreatment period of at least 6 months to a mean of 2.5 events between week 12 and data cutoff (median, 1.8 years of follow-up), according to Pfizer’s press release. Overall, bleeding events were eliminated in 60% of patients who received the one-time infusion vs 29% of patients on factor IX prophylaxis therapy.
Overall, Pfizer reported that the gene therapy was “generally well-tolerated,” with an increase in transaminases reported as the most common adverse event. No deaths, serious infusion reactions, thrombotic events, or development of factor IX antibodies occurred.
Pfizer has said it will continue to monitor patients to assess the therapy’s long-term durability and safety over a 15-year period.
A version of this article appeared on Medscape.com.
<!--$RCSfile: InCopy_agile.xsl,v $ $Revision: 1.35 $-->
<!--$RCSfile: drupal.xsl,v $ $Revision: 1.7 $-->
<root generator="drupal.xsl" gversion="1.7"> <header> <fileName>167870</fileName> <TBEID>0C04FD76.SIG</TBEID> <TBUniqueIdentifier>MD_0C04FD76</TBUniqueIdentifier> <newsOrJournal>News</newsOrJournal> <publisherName>Frontline Medical Communications</publisherName> <storyname/> <articleType>2</articleType> <TBLocation>QC Done-All Pubs</TBLocation> <QCDate>20240426T141633</QCDate> <firstPublished>20240426T141752</firstPublished> <LastPublished>20240426T141752</LastPublished> <pubStatus qcode="stat:"/> <embargoDate/> <killDate/> <CMSDate>20240426T141752</CMSDate> <articleSource/> <facebookInfo/> <meetingNumber/> <byline>M Alex Otto</byline> <bylineText>M. ALEXANDER OTTO, PA, MMS</bylineText> <bylineFull>M. ALEXANDER OTTO, PA, MMS</bylineFull> <bylineTitleText/> <USOrGlobal/> <wireDocType/> <newsDocType/> <journalDocType/> <linkLabel/> <pageRange/> <citation/> <quizID/> <indexIssueDate/> <itemClass qcode="ninat:text"/> <provider qcode="provider:imng"> <name>IMNG Medical Media</name> <rightsInfo> <copyrightHolder> <name>Frontline Medical News</name> </copyrightHolder> <copyrightNotice>Copyright (c) 2015 Frontline Medical News, a Frontline Medical Communications Inc. company. All rights reserved. This material may not be published, broadcast, copied, or otherwise reproduced or distributed without the prior written permission of Frontline Medical Communications Inc.</copyrightNotice> </rightsInfo> </provider> <abstract/> <metaDescription>The US Food and Drug Administration (FDA) has approved the gene therapy fidanacogene elaparvovec (Beqvez) for adults with hemophilia B, a rare bleeding disorder</metaDescription> <articlePDF/> <teaserImage/> <teaser>For adults with hemophilia B, a second gene therapy — also priced at $3.5 million — has been greenlighted by the Food and Drug Administration. </teaser> <title>FDA Approves Second Gene Therapy for Hemophilia B</title> <deck/> <disclaimer/> <AuthorList/> <articleURL/> <doi/> <pubMedID/> <publishXMLStatus/> <publishXMLVersion>1</publishXMLVersion> <useEISSN>0</useEISSN> <urgency/> <pubPubdateYear/> <pubPubdateMonth/> <pubPubdateDay/> <pubVolume/> <pubNumber/> <wireChannels/> <primaryCMSID/> <CMSIDs/> <keywords/> <seeAlsos/> <publications_g> <publicationData> <publicationCode>hemn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> </publications_g> <publications> <term canonical="true">18</term> </publications> <sections> <term canonical="true">37225</term> <term>39313</term> </sections> <topics> <term canonical="true">191</term> </topics> <links/> </header> <itemSet> <newsItem> <itemMeta> <itemRole>Main</itemRole> <itemClass>text</itemClass> <title>FDA Approves Second Gene Therapy for Hemophilia B</title> <deck/> </itemMeta> <itemContent> <p> <span class="tag metaDescription">The US Food and Drug Administration (FDA) has approved the gene therapy <span class="Hyperlink"><a href="https://reference.medscape.com/drug/fidanacogene-elaparvovec-4000393">fidanacogene elaparvovec</a></span> (Beqvez) for adults with <span class="Hyperlink"><a href="https://emedicine.medscape.com/article/779434-overview">hemophilia B</a></span>, a rare bleeding disorder that affects <span class="Hyperlink"><a href="https://www.cdc.gov/ncbddd/hemophilia/features/keyfinding-hemophilia-occurrence-US.html">almost 4 in 100,000 US men.</a></span></span> </p> <p>Patients are eligible for a one-time infusion of Pfizer’s gene therapy if they are currently using clotting <span class="Hyperlink"><a href="https://emedicine.medscape.com/article/779434-overview">factor IX</a></span> prophylaxis therapy; have current or historical life-threatening hemorrhages; or have repeated, serious spontaneous bleeding episodes. <br/><br/>Beqvez is the second gene therapy the agency has approved for hemophilia B, a deficiency in clotting factor IX because of a faulty gene that occurs mostly in males. The <span class="Hyperlink"><a href="https://www.medscape.com/s/viewarticle/984531">FDA approved</a></span> the first gene therapy, <span class="Hyperlink"><a href="https://reference.medscape.com/drug/hemgenix-etranacogene-dezaparvovec-4000307">etranacogene dezaparvovec</a></span> (Hemgenix), in November 2022. <br/><br/>Both therapies deliver a functional copy of the factor IX gene to liver cells via a viral vector. <br/><br/>Pfizer said the list price of Beqvez will be $3.5 million — the same price as Hemgenix. The argument for this hefty price tag is that these gene therapies offer the possibility of a cure whereas ongoing factor IX infusions can cost more than $20 million over a patient’s lifetime. Uptake of Hemgenix, however, has been slow, given the cost and concerns about the therapy’s durability and safety.<br/><br/>Beqvez was approved on the basis of the phase 3 <span class="Hyperlink"><a href="https://www.businesswire.com/news/home/20221229005024/en/Pfizer-Announces-Positive-Top-Line-Results-from-Phase-3-Study-of-Hemophilia-B-Gene-Therapy-Candidate">BENEGENE-2 trial</a></span> in 45 men with moderate to severe hemophilia B. These men had been on factor IX prophylaxis for at least 6 months and had tested negative for antibodies against the viral delivery vector. <br/><br/>The annualized bleeding rate fell from a mean of 4.5 events during the pretreatment period of at least 6 months to a mean of 2.5 events between week 12 and data cutoff (median, 1.8 years of follow-up), according to <span class="Hyperlink"><a href="https://www.pfizer.com/news/press-release/press-release-detail/us-fda-approves-pfizers-beqveztm-fidanacogene-elaparvovec">Pfizer’s press release</a></span>. Overall, bleeding events were eliminated in 60% of patients who received the one-time infusion vs 29% of patients on factor IX prophylaxis therapy.<br/><br/>Overall, Pfizer reported that the gene therapy was “generally well-tolerated,” with an increase in transaminases reported as the most common adverse event. No deaths, serious infusion reactions, thrombotic events, or development of factor IX antibodies occurred. <br/><br/>Pfizer has said it will continue to monitor patients to assess the therapy’s long-term durability and safety over a 15-year period.<span class="end"/></p> <p> <em>A version of this article appeared on <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/fda-approves-second-gene-therapy-hemophilia-b-2024a100086v">Medscape.com</a></span>.</em> </p> </itemContent> </newsItem> <newsItem> <itemMeta> <itemRole>teaser</itemRole> <itemClass>text</itemClass> <title/> <deck/> </itemMeta> <itemContent> </itemContent> </newsItem> </itemSet></root>
Oregon Physician Assistants Get Name Change
On April 4, Oregon’s Governor Tina Kotek signed a bill into law that officially changed the title of “physician assistants” to “physician associates” in the state.
In the Medscape Physician Assistant Career Satisfaction Report 2023, a diverse range of opinions on the title switch was reflected. Only 40% of PAs favored the name change at the time, 45% neither opposed nor favored it, and 15% opposed the name change, reflecting the complexity of the issue.
According to the AAPA, the change came about to better reflect the work PAs do in not just “assisting” physicians but in working independently with patients. Some also felt that the word “assistant” implies dependence. However, despite associate’s more accurate reflection of the job, PAs mostly remain split on whether they want the new moniker.
Many say that the name change will be confusing for the public and their patients, while others say that physician assistant was already not well understood, as patients often thought of the profession as a doctor’s helper or an assistant, like a medical assistant.
Yet many long-time PAs say that they prefer the title they’ve always had and that explaining to patients the new associate title will be equally confusing. Some mentioned patients may think they’re a business associate of the physician.
Oregon PAs won’t immediately switch to the new name. The new law takes effect on June 6, 2024. The Oregon Medical Board will establish regulations and guidance before PAs adopt the new name in their practices.
The law only changes the name of PAs in Oregon, not in other states. In fact, prematurely using the title of physician associate could subject a PA to regulatory challenges or disciplinary actions.
A version of this article appeared on Medscape.com.
On April 4, Oregon’s Governor Tina Kotek signed a bill into law that officially changed the title of “physician assistants” to “physician associates” in the state.
In the Medscape Physician Assistant Career Satisfaction Report 2023, a diverse range of opinions on the title switch was reflected. Only 40% of PAs favored the name change at the time, 45% neither opposed nor favored it, and 15% opposed the name change, reflecting the complexity of the issue.
According to the AAPA, the change came about to better reflect the work PAs do in not just “assisting” physicians but in working independently with patients. Some also felt that the word “assistant” implies dependence. However, despite associate’s more accurate reflection of the job, PAs mostly remain split on whether they want the new moniker.
Many say that the name change will be confusing for the public and their patients, while others say that physician assistant was already not well understood, as patients often thought of the profession as a doctor’s helper or an assistant, like a medical assistant.
Yet many long-time PAs say that they prefer the title they’ve always had and that explaining to patients the new associate title will be equally confusing. Some mentioned patients may think they’re a business associate of the physician.
Oregon PAs won’t immediately switch to the new name. The new law takes effect on June 6, 2024. The Oregon Medical Board will establish regulations and guidance before PAs adopt the new name in their practices.
The law only changes the name of PAs in Oregon, not in other states. In fact, prematurely using the title of physician associate could subject a PA to regulatory challenges or disciplinary actions.
A version of this article appeared on Medscape.com.
On April 4, Oregon’s Governor Tina Kotek signed a bill into law that officially changed the title of “physician assistants” to “physician associates” in the state.
In the Medscape Physician Assistant Career Satisfaction Report 2023, a diverse range of opinions on the title switch was reflected. Only 40% of PAs favored the name change at the time, 45% neither opposed nor favored it, and 15% opposed the name change, reflecting the complexity of the issue.
According to the AAPA, the change came about to better reflect the work PAs do in not just “assisting” physicians but in working independently with patients. Some also felt that the word “assistant” implies dependence. However, despite associate’s more accurate reflection of the job, PAs mostly remain split on whether they want the new moniker.
Many say that the name change will be confusing for the public and their patients, while others say that physician assistant was already not well understood, as patients often thought of the profession as a doctor’s helper or an assistant, like a medical assistant.
Yet many long-time PAs say that they prefer the title they’ve always had and that explaining to patients the new associate title will be equally confusing. Some mentioned patients may think they’re a business associate of the physician.
Oregon PAs won’t immediately switch to the new name. The new law takes effect on June 6, 2024. The Oregon Medical Board will establish regulations and guidance before PAs adopt the new name in their practices.
The law only changes the name of PAs in Oregon, not in other states. In fact, prematurely using the title of physician associate could subject a PA to regulatory challenges or disciplinary actions.
A version of this article appeared on Medscape.com.
<!--$RCSfile: InCopy_agile.xsl,v $ $Revision: 1.35 $-->
<!--$RCSfile: drupal.xsl,v $ $Revision: 1.7 $-->
<root generator="drupal.xsl" gversion="1.7"> <header> <fileName>167861</fileName> <TBEID>0C04FD43.SIG</TBEID> <TBUniqueIdentifier>MD_0C04FD43</TBUniqueIdentifier> <newsOrJournal>News</newsOrJournal> <publisherName>Frontline Medical Communications</publisherName> <storyname/> <articleType>2</articleType> <TBLocation>QC Done-All Pubs</TBLocation> <QCDate>20240426T111340</QCDate> <firstPublished>20240426T114737</firstPublished> <LastPublished>20240426T114737</LastPublished> <pubStatus qcode="stat:"/> <embargoDate/> <killDate/> <CMSDate>20240426T114737</CMSDate> <articleSource/> <facebookInfo/> <meetingNumber/> <byline>Jennifer Nelson</byline> <bylineText>JENNIFER NELSON</bylineText> <bylineFull>JENNIFER NELSON</bylineFull> <bylineTitleText/> <USOrGlobal/> <wireDocType/> <newsDocType>News</newsDocType> <journalDocType/> <linkLabel/> <pageRange/> <citation/> <quizID/> <indexIssueDate/> <itemClass qcode="ninat:text"/> <provider qcode="provider:imng"> <name>IMNG Medical Media</name> <rightsInfo> <copyrightHolder> <name>Frontline Medical News</name> </copyrightHolder> <copyrightNotice>Copyright (c) 2015 Frontline Medical News, a Frontline Medical Communications Inc. company. All rights reserved. This material may not be published, broadcast, copied, or otherwise reproduced or distributed without the prior written permission of Frontline Medical Communications Inc.</copyrightNotice> </rightsInfo> </provider> <abstract/> <metaDescription>The switch is the first of its kind in the United States and comes on the heels of a decision from 2021 by the American Academy of Physician Associates (AAPA) t</metaDescription> <articlePDF/> <teaserImage/> <teaser>In June, Oregon PAs will be referred to as Physician Associates, a title change from Physician Assistants being debated nationwide. </teaser> <title>Oregon Physician Assistants Get Name Change</title> <deck/> <disclaimer/> <AuthorList/> <articleURL/> <doi/> <pubMedID/> <publishXMLStatus/> <publishXMLVersion>1</publishXMLVersion> <useEISSN>0</useEISSN> <urgency/> <pubPubdateYear/> <pubPubdateMonth/> <pubPubdateDay/> <pubVolume/> <pubNumber/> <wireChannels/> <primaryCMSID/> <CMSIDs/> <keywords/> <seeAlsos/> <publications_g> <publicationData> <publicationCode>card</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>chph</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>fp</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>im</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>cpn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>endo</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>skin</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>hemn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>idprac</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>mdsurg</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>nr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle>Neurology Reviews</journalTitle> <journalFullTitle>Neurology Reviews</journalFullTitle> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>ob</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>oncr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>pn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>rn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> </publications_g> <publications> <term>5</term> <term>6</term> <term>15</term> <term canonical="true">21</term> <term>9</term> <term>34</term> <term>13</term> <term>18</term> <term>20</term> <term>52226</term> <term>22</term> <term>23</term> <term>31</term> <term>25</term> <term>26</term> </publications> <sections> <term canonical="true">39313</term> </sections> <topics> <term canonical="true">38029</term> <term>278</term> </topics> <links/> </header> <itemSet> <newsItem> <itemMeta> <itemRole>Main</itemRole> <itemClass>text</itemClass> <title>Oregon Physician Assistants Get Name Change</title> <deck/> </itemMeta> <itemContent> <p>On April 4, Oregon’s Governor Tina Kotek signed a <span class="Hyperlink"><a href="https://www.aapa.org/news-central/2024/04/oregon-governor-tina-kotek-signs-law-changing-pa-title/?utm_source=linkedin&utm_medium=aapa_post&utm_campaign=news_central">bill</a></span> into law that officially changed the title of “physician assistants” to “physician associates” in the state. <span class="tag metaDescription">The switch is the first of its kind in the United States and comes on the heels of a decision from 2021 by the American Academy of Physician Associates (AAPA) to change the meaning of “PA” to “physician associate” from “physician assistant.”</span></p> <p>In the <span class="Hyperlink"><a href="https://www.medscape.com/slideshow/2023-physician-assistant-satisfaction-6016503#2">Medscape Physician Assistant Career Satisfaction Report 2023</a>, </span>a diverse range of opinions on the title switch was reflected. Only 40% of PAs favored the name change at the time, 45% neither opposed nor favored it, and 15% opposed the name change, reflecting the complexity of the issue.<br/><br/>According to the AAPA, the change came about to better reflect the work PAs do in not just “assisting” physicians but in <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/985263">working independently</a></span> with patients. Some also felt that the word “assistant” implies dependence. However, despite associate’s more accurate reflection of the job, PAs mostly remain split on whether they want the new moniker.<br/><br/>Many say that the name change will be confusing for the public and their patients, while others say that physician assistant was already not well understood, as patients often thought of the profession as a doctor’s helper or an assistant, like a medical assistant.<br/><br/>Yet many long-time PAs say that they prefer the title they’ve always had and that explaining to patients the new associate title will be equally confusing. Some mentioned patients may think they’re a business associate of the physician.<br/><br/>Oregon PAs won’t immediately switch to the new name. The new law takes effect on June 6, 2024. The Oregon Medical Board will establish regulations and guidance before PAs adopt the new name in their practices.<br/><br/>The law only changes the name of PAs in Oregon, not in other states. In fact, prematurely using the title of physician associate could subject a PA to regulatory challenges or disciplinary actions.<span class="end"/></p> <p> <em>A version of this article appeared on <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/oregon-physician-assistants-get-name-change-2024a100084h">Medscape.com</a></span>.</em> </p> </itemContent> </newsItem> <newsItem> <itemMeta> <itemRole>teaser</itemRole> <itemClass>text</itemClass> <title/> <deck/> </itemMeta> <itemContent> </itemContent> </newsItem> </itemSet></root>
How These Young MDs Impressed the Hell Out of Their Bosses
Safe to say that anyone undertaking the physician journey does so with intense motivation and book smarts. Still, it can be incredibly hard to stand out. Everyone’s a go-getter, but what’s the X factor?
Here’s what they said ...
Lesson #1: Never Be Scared to Ask
Brien Barnewolt, MD, chairman and chief of the Department of Emergency Medicine at Tufts Medical Center, was very much surprised when a resident named Scott G. Weiner did something unexpected: Go after a job in the fall of his junior year residency instead of following the typical senior year trajectory.
“It’s very unusual for a trainee to apply for a job virtually a year ahead of schedule. But he knew what he wanted,” said Dr. Barnewolt. “I’d never had anybody come to me in that same scenario, and I’ve been doing this a long time.”
Under normal circumstances it would’ve been easy for Dr. Barnewolt to say no. But the unexpected request made him and his colleagues take a closer look, and they were impressed with Dr. Weiner’s skills. That, paired with his ambition and demeanor, compelled them to offer him an early job. But there’s more.
As the next year approached, Dr. Weiner explained he had an opportunity to work in emergency medicine in Tuscany and asked if he could take a 1-year delayed start for the position he applied a year early for.
The department held his position, and upon his return, Dr. Weiner made a lasting impact at Tufts before eventually moving on. “He outgrew us, which is nice to see,” Dr. Barnewolt said. (Dr. Weiner is currently McGraw Distinguished Chair in Emergency Medicine at Brigham and Women’s Hospital and associate professor at Harvard Medical School.)
Bottom line: Why did Dr. Barnewolt and his colleagues do so much to accommodate a young candidate? Yes, Dr. Weiner was talented, but he was also up-front about his ambitions from the get-go. Dr. Barnewolt said that kind of initiative can only be looked at positively.
“My advice would be, if you see an opportunity or a potential place where you might want to work, put out those feelers, start those conversations,” he said. “It’s not too early, especially in certain specialties, where the job market is very tight. Then, when circumstances change, be open about it and have that conversation. The worst that somebody can say is no, so it never hurts to be honest and open about where you want to go and what you want to be.”
Lesson #2: Chase Your Passion ‘Relentlessly’
Vance G. Fowler, MD, MHS, an infectious disease specialist at Duke University School of Medicine, runs a laboratory that researches methicillin-resistant Staphylococcus aureus (MRSA). Over the years, he’s mentored many doctors but understands the ambitions of young trainees don’t always align with the little free time that they have. “Many of them drop away when you give them a [side] project,” he said.
So when Tori Kinamon asked him to work on an MRSA project — in her first year — he gave her one that focused on researching vertebral osteomyelitis, a bone infection that can coincide with S aureus. What Dr. Fowler didn’t know: Kinamon (now MD) had been a competitive gymnast at Brown and battled her own life-threatening infection with MRSA.
“To my absolute astonishment, not only did she stick to it, but she was able to compile a presentation on the science and gave an oral presentation within a year of walking in the door,” said Dr. Fowler.
She went on to lead an initiative between the National Institutes of Health and US Food and Drug Administration to create endpoints for clinical drug trials, all of which occurred before starting her residency, which she’s about to embark upon.
Dr. Kinamon’s a good example, he said, of what happens when you add genuine passion to book smarts. Those who do always stand out because you can’t fake that. “Find your passion, and then chase it down relentlessly,” he said. “Once you’ve found your passion, things get easy because it stops being work and it starts being something else.”
If you haven’t identified a focus area, Dr. Fowler said to “be agnostic and observant. Keep your eyes open and your options open because you may surprise yourself. It may turn out that you end up liking something a whole lot more than you thought you did.”
Lesson #3: When You Say You’ve Always Wanted to Do Something, Do Something
As the chief of pulmonary and critical care medicine at the Northwestern Medicine Canning Thoracic Institute, Scott Budinger, MD, often hears lip service from doctors who want to put their skills to use in their local communities. One of his students actually did it.
Justin Fiala, MD, a pulmonary, critical care, and sleep specialist at Northwestern Medicine, joined Northwestern as a pulmonary fellow with a big interest in addressing health equity issues.
Dr. Fiala began volunteering with CommunityHealth during his fellowship and saw that many patients of the free Chicago-area clinic needed help with sleep disorders. He launched the organization’s first sleep clinic and its Patient-Centered Apnea Protocols Initiative.
“He developed a plan with some of the partners of the sleep apnea equipment to do home sleep testing for these patients that’s free of cost,” said Dr. Budinger.
Dr. Fiala goes in on Saturdays and runs a free clinic conducting sleep studies for patients and outfits them with devices that they need to improve their conditions, said Dr. Budinger.
“And these patients are the severest of the severe patients,” he said. “These are people that have severe sleep apnea that are driving around the roads, oftentimes don’t have insurance because they’re also precluded from having auto insurance. So, this is really something that not just benefits these patients but benefits our whole community.”
The fact that Dr. Fiala followed through on something that all doctors aspire to do — and in the middle of a very busy training program — is something that Dr. Budinger said makes him stand out in a big way.
“If you talk to any of our trainees or young faculty, everybody’s interested in addressing the issue of health disparities,” said Dr. Budinger. “Justin looked at that and said, ‘Well, you know, I’m not interested in talking about it. What can I do about this problem? And how can I actually get boots on the ground and help?’ That requires a big activation energy that many people don’t have.”
Lesson #4: Be a People-Person and a Patient-Person
When hiring employees at American Family Care in Portland, Oregon, Andrew Miller, MD, director of provider training, is always on the lookout for young MDs with emotional intelligence and a good bedside manner. He has been recently blown away, however, by a young physician’s assistant named Joseph Van Bindsbergen, PA-C, who was described as “all-around wonderful” during his reference check.
“Having less than 6 months of experience out of school, he is our highest ranked provider, whether it’s a nurse practitioner, PA, or doctor, in terms of patient satisfaction,” said Dr. Miller. The young PA has an “unprecedented perfect score” on his NPS rating.
Why? Patients said they’ve never felt as heard as they felt with Van Bindsbergen.
“That’s the thing I think that the up-and-coming providers should be focusing on is making your patients feel heard,” explained Dr. Miller. Van Bindsbergen is great at building rapport with a patient, whether they are 6 or 96. “He doesn’t just ask about sore throat symptoms. He asks, ‘what is the impact on your life of the sore throat? How does it affect your family or your work? What do you think this could be besides just strep? What are your concerns?’ ”
Dr. Miller said the magic of Van Bindsbergen is that he has an innate ability to look at patients “not just as a diagnosis but as a person, which they love.”
Lesson #5: Remember to Make That Difference With Each Patient
Doctors are used to swooping in and seeing a patient, ordering further testing if needed, and then moving on to the next patient. But one young intern at the start of his medical career broke this mold by giving a very anxious patient some much-needed support.
“There was a resident who was working overnight, and this poor young woman came in who had a new diagnosis of an advanced illness and a lot of anxiety around her condition, the newness of it, and the impact this is going to have on her family and her life,” said Elizabeth Horn Prsic, MD, assistant professor at Yale School of Medicine and firm chief for medical oncology and the director of Adult Inpatient Palliative Care.
Dr. Prsic found out the next morning that this trainee accompanied the patient to the MRI and held her hand as much as he was allowed to throughout the entire experience. “I was like, ‘wait you went down with her to radiology?’ And he’s like, ‘Yes, I was there the whole time,’ ” she recalled.
This gesture not only helped the patient feel calmer after receiving a potentially life-altering diagnosis but also helped ensure the test results were as clear as possible.
“If the study is not done well and a patient is moving or uncomfortable, it has to be stopped early or paused,” said Dr. Prsic. “Then the study is not very useful. In situations like these, medical decisions may be made based on imperfect data. The fact that we had this full complete good quality scan helped us get the care that she needed in a much timelier manner to help her and to move along the care that she that was medically appropriate for her.”
Dr. Prsic got emotional reflecting on the experience. Working at Yale, she saw a ton of intelligent doctors come through the ranks. But this gesture, she said, should serve as a reminder that “you don’t need to be the smartest person in the room to just be there for a patient. It was pure empathic presence and human connection. It gave me hope in the next generation of physicians.”
A version of this article appeared on Medscape.com.
Safe to say that anyone undertaking the physician journey does so with intense motivation and book smarts. Still, it can be incredibly hard to stand out. Everyone’s a go-getter, but what’s the X factor?
Here’s what they said ...
Lesson #1: Never Be Scared to Ask
Brien Barnewolt, MD, chairman and chief of the Department of Emergency Medicine at Tufts Medical Center, was very much surprised when a resident named Scott G. Weiner did something unexpected: Go after a job in the fall of his junior year residency instead of following the typical senior year trajectory.
“It’s very unusual for a trainee to apply for a job virtually a year ahead of schedule. But he knew what he wanted,” said Dr. Barnewolt. “I’d never had anybody come to me in that same scenario, and I’ve been doing this a long time.”
Under normal circumstances it would’ve been easy for Dr. Barnewolt to say no. But the unexpected request made him and his colleagues take a closer look, and they were impressed with Dr. Weiner’s skills. That, paired with his ambition and demeanor, compelled them to offer him an early job. But there’s more.
As the next year approached, Dr. Weiner explained he had an opportunity to work in emergency medicine in Tuscany and asked if he could take a 1-year delayed start for the position he applied a year early for.
The department held his position, and upon his return, Dr. Weiner made a lasting impact at Tufts before eventually moving on. “He outgrew us, which is nice to see,” Dr. Barnewolt said. (Dr. Weiner is currently McGraw Distinguished Chair in Emergency Medicine at Brigham and Women’s Hospital and associate professor at Harvard Medical School.)
Bottom line: Why did Dr. Barnewolt and his colleagues do so much to accommodate a young candidate? Yes, Dr. Weiner was talented, but he was also up-front about his ambitions from the get-go. Dr. Barnewolt said that kind of initiative can only be looked at positively.
“My advice would be, if you see an opportunity or a potential place where you might want to work, put out those feelers, start those conversations,” he said. “It’s not too early, especially in certain specialties, where the job market is very tight. Then, when circumstances change, be open about it and have that conversation. The worst that somebody can say is no, so it never hurts to be honest and open about where you want to go and what you want to be.”
Lesson #2: Chase Your Passion ‘Relentlessly’
Vance G. Fowler, MD, MHS, an infectious disease specialist at Duke University School of Medicine, runs a laboratory that researches methicillin-resistant Staphylococcus aureus (MRSA). Over the years, he’s mentored many doctors but understands the ambitions of young trainees don’t always align with the little free time that they have. “Many of them drop away when you give them a [side] project,” he said.
So when Tori Kinamon asked him to work on an MRSA project — in her first year — he gave her one that focused on researching vertebral osteomyelitis, a bone infection that can coincide with S aureus. What Dr. Fowler didn’t know: Kinamon (now MD) had been a competitive gymnast at Brown and battled her own life-threatening infection with MRSA.
“To my absolute astonishment, not only did she stick to it, but she was able to compile a presentation on the science and gave an oral presentation within a year of walking in the door,” said Dr. Fowler.
She went on to lead an initiative between the National Institutes of Health and US Food and Drug Administration to create endpoints for clinical drug trials, all of which occurred before starting her residency, which she’s about to embark upon.
Dr. Kinamon’s a good example, he said, of what happens when you add genuine passion to book smarts. Those who do always stand out because you can’t fake that. “Find your passion, and then chase it down relentlessly,” he said. “Once you’ve found your passion, things get easy because it stops being work and it starts being something else.”
If you haven’t identified a focus area, Dr. Fowler said to “be agnostic and observant. Keep your eyes open and your options open because you may surprise yourself. It may turn out that you end up liking something a whole lot more than you thought you did.”
Lesson #3: When You Say You’ve Always Wanted to Do Something, Do Something
As the chief of pulmonary and critical care medicine at the Northwestern Medicine Canning Thoracic Institute, Scott Budinger, MD, often hears lip service from doctors who want to put their skills to use in their local communities. One of his students actually did it.
Justin Fiala, MD, a pulmonary, critical care, and sleep specialist at Northwestern Medicine, joined Northwestern as a pulmonary fellow with a big interest in addressing health equity issues.
Dr. Fiala began volunteering with CommunityHealth during his fellowship and saw that many patients of the free Chicago-area clinic needed help with sleep disorders. He launched the organization’s first sleep clinic and its Patient-Centered Apnea Protocols Initiative.
“He developed a plan with some of the partners of the sleep apnea equipment to do home sleep testing for these patients that’s free of cost,” said Dr. Budinger.
Dr. Fiala goes in on Saturdays and runs a free clinic conducting sleep studies for patients and outfits them with devices that they need to improve their conditions, said Dr. Budinger.
“And these patients are the severest of the severe patients,” he said. “These are people that have severe sleep apnea that are driving around the roads, oftentimes don’t have insurance because they’re also precluded from having auto insurance. So, this is really something that not just benefits these patients but benefits our whole community.”
The fact that Dr. Fiala followed through on something that all doctors aspire to do — and in the middle of a very busy training program — is something that Dr. Budinger said makes him stand out in a big way.
“If you talk to any of our trainees or young faculty, everybody’s interested in addressing the issue of health disparities,” said Dr. Budinger. “Justin looked at that and said, ‘Well, you know, I’m not interested in talking about it. What can I do about this problem? And how can I actually get boots on the ground and help?’ That requires a big activation energy that many people don’t have.”
Lesson #4: Be a People-Person and a Patient-Person
When hiring employees at American Family Care in Portland, Oregon, Andrew Miller, MD, director of provider training, is always on the lookout for young MDs with emotional intelligence and a good bedside manner. He has been recently blown away, however, by a young physician’s assistant named Joseph Van Bindsbergen, PA-C, who was described as “all-around wonderful” during his reference check.
“Having less than 6 months of experience out of school, he is our highest ranked provider, whether it’s a nurse practitioner, PA, or doctor, in terms of patient satisfaction,” said Dr. Miller. The young PA has an “unprecedented perfect score” on his NPS rating.
Why? Patients said they’ve never felt as heard as they felt with Van Bindsbergen.
“That’s the thing I think that the up-and-coming providers should be focusing on is making your patients feel heard,” explained Dr. Miller. Van Bindsbergen is great at building rapport with a patient, whether they are 6 or 96. “He doesn’t just ask about sore throat symptoms. He asks, ‘what is the impact on your life of the sore throat? How does it affect your family or your work? What do you think this could be besides just strep? What are your concerns?’ ”
Dr. Miller said the magic of Van Bindsbergen is that he has an innate ability to look at patients “not just as a diagnosis but as a person, which they love.”
Lesson #5: Remember to Make That Difference With Each Patient
Doctors are used to swooping in and seeing a patient, ordering further testing if needed, and then moving on to the next patient. But one young intern at the start of his medical career broke this mold by giving a very anxious patient some much-needed support.
“There was a resident who was working overnight, and this poor young woman came in who had a new diagnosis of an advanced illness and a lot of anxiety around her condition, the newness of it, and the impact this is going to have on her family and her life,” said Elizabeth Horn Prsic, MD, assistant professor at Yale School of Medicine and firm chief for medical oncology and the director of Adult Inpatient Palliative Care.
Dr. Prsic found out the next morning that this trainee accompanied the patient to the MRI and held her hand as much as he was allowed to throughout the entire experience. “I was like, ‘wait you went down with her to radiology?’ And he’s like, ‘Yes, I was there the whole time,’ ” she recalled.
This gesture not only helped the patient feel calmer after receiving a potentially life-altering diagnosis but also helped ensure the test results were as clear as possible.
“If the study is not done well and a patient is moving or uncomfortable, it has to be stopped early or paused,” said Dr. Prsic. “Then the study is not very useful. In situations like these, medical decisions may be made based on imperfect data. The fact that we had this full complete good quality scan helped us get the care that she needed in a much timelier manner to help her and to move along the care that she that was medically appropriate for her.”
Dr. Prsic got emotional reflecting on the experience. Working at Yale, she saw a ton of intelligent doctors come through the ranks. But this gesture, she said, should serve as a reminder that “you don’t need to be the smartest person in the room to just be there for a patient. It was pure empathic presence and human connection. It gave me hope in the next generation of physicians.”
A version of this article appeared on Medscape.com.
Safe to say that anyone undertaking the physician journey does so with intense motivation and book smarts. Still, it can be incredibly hard to stand out. Everyone’s a go-getter, but what’s the X factor?
Here’s what they said ...
Lesson #1: Never Be Scared to Ask
Brien Barnewolt, MD, chairman and chief of the Department of Emergency Medicine at Tufts Medical Center, was very much surprised when a resident named Scott G. Weiner did something unexpected: Go after a job in the fall of his junior year residency instead of following the typical senior year trajectory.
“It’s very unusual for a trainee to apply for a job virtually a year ahead of schedule. But he knew what he wanted,” said Dr. Barnewolt. “I’d never had anybody come to me in that same scenario, and I’ve been doing this a long time.”
Under normal circumstances it would’ve been easy for Dr. Barnewolt to say no. But the unexpected request made him and his colleagues take a closer look, and they were impressed with Dr. Weiner’s skills. That, paired with his ambition and demeanor, compelled them to offer him an early job. But there’s more.
As the next year approached, Dr. Weiner explained he had an opportunity to work in emergency medicine in Tuscany and asked if he could take a 1-year delayed start for the position he applied a year early for.
The department held his position, and upon his return, Dr. Weiner made a lasting impact at Tufts before eventually moving on. “He outgrew us, which is nice to see,” Dr. Barnewolt said. (Dr. Weiner is currently McGraw Distinguished Chair in Emergency Medicine at Brigham and Women’s Hospital and associate professor at Harvard Medical School.)
Bottom line: Why did Dr. Barnewolt and his colleagues do so much to accommodate a young candidate? Yes, Dr. Weiner was talented, but he was also up-front about his ambitions from the get-go. Dr. Barnewolt said that kind of initiative can only be looked at positively.
“My advice would be, if you see an opportunity or a potential place where you might want to work, put out those feelers, start those conversations,” he said. “It’s not too early, especially in certain specialties, where the job market is very tight. Then, when circumstances change, be open about it and have that conversation. The worst that somebody can say is no, so it never hurts to be honest and open about where you want to go and what you want to be.”
Lesson #2: Chase Your Passion ‘Relentlessly’
Vance G. Fowler, MD, MHS, an infectious disease specialist at Duke University School of Medicine, runs a laboratory that researches methicillin-resistant Staphylococcus aureus (MRSA). Over the years, he’s mentored many doctors but understands the ambitions of young trainees don’t always align with the little free time that they have. “Many of them drop away when you give them a [side] project,” he said.
So when Tori Kinamon asked him to work on an MRSA project — in her first year — he gave her one that focused on researching vertebral osteomyelitis, a bone infection that can coincide with S aureus. What Dr. Fowler didn’t know: Kinamon (now MD) had been a competitive gymnast at Brown and battled her own life-threatening infection with MRSA.
“To my absolute astonishment, not only did she stick to it, but she was able to compile a presentation on the science and gave an oral presentation within a year of walking in the door,” said Dr. Fowler.
She went on to lead an initiative between the National Institutes of Health and US Food and Drug Administration to create endpoints for clinical drug trials, all of which occurred before starting her residency, which she’s about to embark upon.
Dr. Kinamon’s a good example, he said, of what happens when you add genuine passion to book smarts. Those who do always stand out because you can’t fake that. “Find your passion, and then chase it down relentlessly,” he said. “Once you’ve found your passion, things get easy because it stops being work and it starts being something else.”
If you haven’t identified a focus area, Dr. Fowler said to “be agnostic and observant. Keep your eyes open and your options open because you may surprise yourself. It may turn out that you end up liking something a whole lot more than you thought you did.”
Lesson #3: When You Say You’ve Always Wanted to Do Something, Do Something
As the chief of pulmonary and critical care medicine at the Northwestern Medicine Canning Thoracic Institute, Scott Budinger, MD, often hears lip service from doctors who want to put their skills to use in their local communities. One of his students actually did it.
Justin Fiala, MD, a pulmonary, critical care, and sleep specialist at Northwestern Medicine, joined Northwestern as a pulmonary fellow with a big interest in addressing health equity issues.
Dr. Fiala began volunteering with CommunityHealth during his fellowship and saw that many patients of the free Chicago-area clinic needed help with sleep disorders. He launched the organization’s first sleep clinic and its Patient-Centered Apnea Protocols Initiative.
“He developed a plan with some of the partners of the sleep apnea equipment to do home sleep testing for these patients that’s free of cost,” said Dr. Budinger.
Dr. Fiala goes in on Saturdays and runs a free clinic conducting sleep studies for patients and outfits them with devices that they need to improve their conditions, said Dr. Budinger.
“And these patients are the severest of the severe patients,” he said. “These are people that have severe sleep apnea that are driving around the roads, oftentimes don’t have insurance because they’re also precluded from having auto insurance. So, this is really something that not just benefits these patients but benefits our whole community.”
The fact that Dr. Fiala followed through on something that all doctors aspire to do — and in the middle of a very busy training program — is something that Dr. Budinger said makes him stand out in a big way.
“If you talk to any of our trainees or young faculty, everybody’s interested in addressing the issue of health disparities,” said Dr. Budinger. “Justin looked at that and said, ‘Well, you know, I’m not interested in talking about it. What can I do about this problem? And how can I actually get boots on the ground and help?’ That requires a big activation energy that many people don’t have.”
Lesson #4: Be a People-Person and a Patient-Person
When hiring employees at American Family Care in Portland, Oregon, Andrew Miller, MD, director of provider training, is always on the lookout for young MDs with emotional intelligence and a good bedside manner. He has been recently blown away, however, by a young physician’s assistant named Joseph Van Bindsbergen, PA-C, who was described as “all-around wonderful” during his reference check.
“Having less than 6 months of experience out of school, he is our highest ranked provider, whether it’s a nurse practitioner, PA, or doctor, in terms of patient satisfaction,” said Dr. Miller. The young PA has an “unprecedented perfect score” on his NPS rating.
Why? Patients said they’ve never felt as heard as they felt with Van Bindsbergen.
“That’s the thing I think that the up-and-coming providers should be focusing on is making your patients feel heard,” explained Dr. Miller. Van Bindsbergen is great at building rapport with a patient, whether they are 6 or 96. “He doesn’t just ask about sore throat symptoms. He asks, ‘what is the impact on your life of the sore throat? How does it affect your family or your work? What do you think this could be besides just strep? What are your concerns?’ ”
Dr. Miller said the magic of Van Bindsbergen is that he has an innate ability to look at patients “not just as a diagnosis but as a person, which they love.”
Lesson #5: Remember to Make That Difference With Each Patient
Doctors are used to swooping in and seeing a patient, ordering further testing if needed, and then moving on to the next patient. But one young intern at the start of his medical career broke this mold by giving a very anxious patient some much-needed support.
“There was a resident who was working overnight, and this poor young woman came in who had a new diagnosis of an advanced illness and a lot of anxiety around her condition, the newness of it, and the impact this is going to have on her family and her life,” said Elizabeth Horn Prsic, MD, assistant professor at Yale School of Medicine and firm chief for medical oncology and the director of Adult Inpatient Palliative Care.
Dr. Prsic found out the next morning that this trainee accompanied the patient to the MRI and held her hand as much as he was allowed to throughout the entire experience. “I was like, ‘wait you went down with her to radiology?’ And he’s like, ‘Yes, I was there the whole time,’ ” she recalled.
This gesture not only helped the patient feel calmer after receiving a potentially life-altering diagnosis but also helped ensure the test results were as clear as possible.
“If the study is not done well and a patient is moving or uncomfortable, it has to be stopped early or paused,” said Dr. Prsic. “Then the study is not very useful. In situations like these, medical decisions may be made based on imperfect data. The fact that we had this full complete good quality scan helped us get the care that she needed in a much timelier manner to help her and to move along the care that she that was medically appropriate for her.”
Dr. Prsic got emotional reflecting on the experience. Working at Yale, she saw a ton of intelligent doctors come through the ranks. But this gesture, she said, should serve as a reminder that “you don’t need to be the smartest person in the room to just be there for a patient. It was pure empathic presence and human connection. It gave me hope in the next generation of physicians.”
A version of this article appeared on Medscape.com.
<!--$RCSfile: InCopy_agile.xsl,v $ $Revision: 1.35 $-->
<!--$RCSfile: drupal.xsl,v $ $Revision: 1.7 $-->
<root generator="drupal.xsl" gversion="1.7"> <header> <fileName>167845</fileName> <TBEID>0C04FCA7.SIG</TBEID> <TBUniqueIdentifier>MD_0C04FCA7</TBUniqueIdentifier> <newsOrJournal>News</newsOrJournal> <publisherName>Frontline Medical Communications</publisherName> <storyname/> <articleType>2</articleType> <TBLocation>QC Done-All Pubs</TBLocation> <QCDate>20240424T155925</QCDate> <firstPublished>20240424T155933</firstPublished> <LastPublished>20240424T155933</LastPublished> <pubStatus qcode="stat:"/> <embargoDate/> <killDate/> <CMSDate>20240424T155933</CMSDate> <articleSource/> <facebookInfo/> <meetingNumber/> <byline>Nicole Pajer</byline> <bylineText>NICOLE PAJER</bylineText> <bylineFull>NICOLE PAJER</bylineFull> <bylineTitleText/> <USOrGlobal/> <wireDocType/> <newsDocType>News</newsDocType> <journalDocType/> <linkLabel/> <pageRange/> <citation/> <quizID/> <indexIssueDate/> <itemClass qcode="ninat:text"/> <provider qcode="provider:imng"> <name>IMNG Medical Media</name> <rightsInfo> <copyrightHolder> <name>Frontline Medical News</name> </copyrightHolder> <copyrightNotice>Copyright (c) 2015 Frontline Medical News, a Frontline Medical Communications Inc. company. All rights reserved. This material may not be published, broadcast, copied, or otherwise reproduced or distributed without the prior written permission of Frontline Medical Communications Inc.</copyrightNotice> </rightsInfo> </provider> <abstract/> <metaDescription>We asked five veteran doctors who have supervised scores of young medical professionals over the years to tell us about that one person who impressed the hell o</metaDescription> <articlePDF/> <teaserImage/> <teaser>Young doctors who got noticed shared their goals, followed through on their career passions, and made patients feel heard.</teaser> <title>How These Young MDs Impressed the Hell Out of Their Bosses</title> <deck/> <disclaimer/> <AuthorList/> <articleURL/> <doi/> <pubMedID/> <publishXMLStatus/> <publishXMLVersion>1</publishXMLVersion> <useEISSN>0</useEISSN> <urgency/> <pubPubdateYear/> <pubPubdateMonth/> <pubPubdateDay/> <pubVolume/> <pubNumber/> <wireChannels/> <primaryCMSID/> <CMSIDs/> <keywords/> <seeAlsos/> <publications_g> <publicationData> <publicationCode>chph</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>im</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>idprac</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>fp</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>oncr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>pn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>ob</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>mdsurg</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>hemn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>skin</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>endo</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>card</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> </publications_g> <publications> <term>6</term> <term canonical="true">21</term> <term>20</term> <term>15</term> <term>31</term> <term>25</term> <term>23</term> <term>52226</term> <term>18</term> <term>13</term> <term>34</term> <term>5</term> </publications> <sections> <term canonical="true">39313</term> </sections> <topics> <term canonical="true">38029</term> <term>278</term> </topics> <links/> </header> <itemSet> <newsItem> <itemMeta> <itemRole>Main</itemRole> <itemClass>text</itemClass> <title>How These Young MDs Impressed the Hell Out of Their Bosses</title> <deck/> </itemMeta> <itemContent> <p>Safe to say that anyone undertaking the physician journey does so with intense motivation and book smarts. Still, it can be incredibly hard to stand out. Everyone’s a go-getter, but what’s the X factor?</p> <p><span class="tag metaDescription">We asked five veteran doctors who have supervised scores of young medical professionals over the years to tell us about that one person who impressed the hell out of them — what they did, why it made them game changers, and what every doctor can learn from them.</span> Here’s what they said ...<br/><br/></p> <h2>Lesson #1: Never Be Scared to Ask</h2> <p><span class="Hyperlink"><a href="https://www.tuftsmedicine.org/doctor/brien-barnewolt">Brien Barnewolt, MD</a></span>, chairman and chief of the Department of Emergency Medicine at Tufts Medical Center, was very much surprised when a resident named Scott G. Weiner did something unexpected: Go after a job in the fall of his junior year residency instead of following the typical senior year trajectory.<br/><br/>“It’s very unusual for a trainee to apply for a job virtually a year ahead of schedule. But he knew what he wanted,” said Dr. Barnewolt. “I’d never had anybody come to me in that same scenario, and I’ve been doing this a long time.”<br/><br/>Under normal circumstances it would’ve been easy for Dr. Barnewolt to say no. But the unexpected request made him and his colleagues take a closer look, and they were impressed with Dr. Weiner’s skills. That, paired with his ambition and demeanor, compelled them to offer him an early job. But there’s more.<br/><br/>As the next year approached, Dr. Weiner explained he had an opportunity to work in emergency medicine in Tuscany and asked if he could take a 1-year delayed start for the position he applied a year early for.<br/><br/>The department held his position, and upon his return, Dr. Weiner made a lasting impact at Tufts before eventually moving on. “He outgrew us, which is nice to see,” Dr. Barnewolt said. (<span class="Hyperlink"><a href="https://physiciandirectory.brighamandwomens.org/details/12465/scott-weiner-emergency_medicine-boston">Dr. Weiner is currently</a></span> McGraw Distinguished Chair in Emergency Medicine at Brigham and Women’s Hospital and associate professor at Harvard Medical School.)<br/><br/>Bottom line: Why did Dr. Barnewolt and his colleagues do so much to accommodate a young candidate? Yes, Dr. Weiner was talented, but he was also up-front about his ambitions from the get-go. Dr. Barnewolt said that kind of initiative can only be looked at positively.<br/><br/>“My advice would be, if you see an opportunity or a potential place where you might want to work, put out those feelers, start those conversations,” he said. “It’s not too early, especially in certain specialties, where the job market is very tight. Then, when circumstances change, be open about it and have that conversation. The worst that somebody can say is no, so it never hurts to be honest and open about where you want to go and what you want to be.”<br/><br/></p> <h2>Lesson #2: Chase Your Passion ‘Relentlessly’</h2> <p><span class="Hyperlink"><a href="https://medicine.duke.edu/profile/vance-garrison-fowler">Vance G. Fowler, MD, MHS</a></span>, an infectious disease specialist at Duke University School of Medicine, runs a laboratory that researches methicillin-resistant <em>Staphylococcus aureus</em> (MRSA). Over the years, he’s mentored many doctors but understands the ambitions of young trainees don’t always align with the little free time that they have. “Many of them drop away when you give them a [side] project,” he said.<br/><br/>So when <span class="Hyperlink"><a href="https://medschool.duke.edu/stories/fighting-chance-against-infection">Tori Kinamon</a></span> asked him to work on an MRSA project — in her first year — he gave her one that focused on researching vertebral <span class="Hyperlink">osteomyelitis</span>, a bone infection that can coincide with <em>S aureus</em>. What Dr. Fowler didn’t know: Kinamon (now MD) had been a competitive gymnast at Brown and battled her own life-threatening infection with MRSA.<br/><br/>“To my absolute astonishment, not only did she stick to it, but she was able to compile a presentation on the science and gave an oral presentation within a year of walking in the door,” said Dr. Fowler.<br/><br/>She went on to lead an initiative between the National Institutes of Health and US Food and Drug Administration to create endpoints for clinical drug trials, all of which occurred before starting her residency, which she’s about to embark upon.<br/><br/>Dr. Kinamon’s a good example, he said, of what happens when you add genuine passion to book smarts. Those who do always stand out because you can’t fake that. “Find your passion, and then chase it down relentlessly,” he said. “Once you’ve found your passion, things get easy because it stops being work and it starts being something else.”<br/><br/>If you haven’t identified a focus area, Dr. Fowler said to “be agnostic and observant. Keep your eyes open and your options open because you may surprise yourself. It may turn out that you end up liking something a whole lot more than you thought you did.”<br/><br/></p> <h2>Lesson #3: When You Say You’ve Always Wanted to Do Something, Do Something</h2> <p>As the chief of pulmonary and critical care medicine at the Northwestern Medicine Canning Thoracic Institute, <span class="Hyperlink"><a href="https://www.feinberg.northwestern.edu/faculty-profiles/az/profile.html?xid=10309">Scott Budinger, MD,</a></span> often hears lip service from doctors who want to put their skills to use in their local communities. One of his students actually did it. <br/><br/><span class="Hyperlink"><a href="https://www.nm.org/doctors/1760821474/justin-anthony-fiala-md">Justin Fiala, MD</a></span>, a pulmonary, critical care, and sleep specialist at Northwestern Medicine, joined Northwestern as a pulmonary fellow with a big interest in addressing health equity issues.<br/><br/>Dr. Fiala began volunteering with CommunityHealth during his fellowship and saw that many patients of the free Chicago-area clinic needed help with sleep disorders. He launched the organization’s first sleep clinic and its Patient-Centered Apnea Protocols Initiative.<br/><br/>“He developed a plan with some of the partners of the sleep apnea equipment to do home sleep testing for these patients that’s free of cost,” said Dr. Budinger.<br/><br/>Dr. Fiala goes in on Saturdays and runs a free clinic conducting sleep studies for patients and outfits them with devices that they need to improve their conditions, said Dr. Budinger.<br/><br/>“And these patients are the severest of the severe patients,” he said. “These are people that have severe sleep apnea that are driving around the roads, oftentimes don’t have insurance because they’re also precluded from having auto insurance. So, this is really something that not just benefits these patients but benefits our whole community.”<br/><br/>The fact that Dr. Fiala followed through on something that all doctors aspire to do — and in the middle of a very busy training program — is something that Dr. Budinger said makes him stand out in a big way.<br/><br/>“If you talk to any of our trainees or young faculty, everybody’s interested in addressing the issue of health disparities,” said Dr. Budinger. “Justin looked at that and said, ‘Well, you know, I’m not interested in talking about it. What can I do about this problem? And how can I actually get boots on the ground and help?’ That requires a big activation energy that many people don’t have.”<br/><br/></p> <h2>Lesson #4: Be a People-Person and a Patient-Person</h2> <p>When hiring employees at American Family Care in Portland, Oregon, Andrew Miller, MD, director of provider training, is always on the lookout for young MDs with emotional intelligence and a good bedside manner. He has been recently blown away, however, by a young physician’s assistant named Joseph Van Bindsbergen, PA-C, who was described as “all-around wonderful” during his reference check.<br/><br/>“Having less than 6 months of experience out of school, he is our highest ranked provider, whether it’s a nurse practitioner, PA, or doctor, in terms of patient satisfaction,” said Dr. Miller. The young PA has an “unprecedented perfect score” on his NPS rating.<br/><br/>Why? Patients said they’ve never felt as heard as they felt with Van Bindsbergen.<br/><br/>“That’s the thing I think that the up-and-coming providers should be focusing on is making your patients feel heard,” explained Dr. Miller. Van Bindsbergen is great at building rapport with a patient, whether they are 6 or 96. “He doesn’t just ask about sore throat symptoms. He asks, ‘what is the impact on your life of the sore throat? How does it affect your family or your work? What do you think this could be besides just strep? What are your concerns?’ ”<br/><br/>Dr. Miller said the magic of Van Bindsbergen is that he has an innate ability to look at patients “not just as a diagnosis but as a person, which they love.”<br/><br/></p> <h2>Lesson #5: Remember to Make That Difference With Each Patient</h2> <p>Doctors are used to swooping in and seeing a patient, ordering further testing if needed, and then moving on to the next patient. But one young intern at the start of his medical career broke this mold by giving a very anxious patient some much-needed support.<br/><br/>“There was a resident who was working overnight, and this poor young woman came in who had a new diagnosis of an advanced illness and a lot of anxiety around her condition, the newness of it, and the impact this is going to have on her family and her life,” said <span class="Hyperlink"><a href="https://medicine.yale.edu/profile/elizabeth-prsic/">Elizabeth Horn Prsic, MD</a></span>, assistant professor at Yale School of Medicine and firm chief for medical oncology and the director of Adult Inpatient Palliative Care.<br/><br/>Dr. Prsic found out the next morning that this trainee accompanied the patient to the MRI and held her hand as much as he was allowed to throughout the entire experience. “I was like, ‘wait you went down with her to radiology?’ And he’s like, ‘Yes, I was there the whole time,’ ” she recalled.<br/><br/>This gesture not only helped the patient feel calmer after receiving a potentially life-altering diagnosis but also helped ensure the test results were as clear as possible.<br/><br/>“If the study is not done well and a patient is moving or uncomfortable, it has to be stopped early or paused,” said Dr. Prsic. “Then the study is not very useful. In situations like these, medical decisions may be made based on imperfect data. The fact that we had this full complete good quality scan helped us get the care that she needed in a much timelier manner to help her and to move along the care that she that was medically appropriate for her.”<br/><br/>Dr. Prsic got emotional reflecting on the experience. Working at Yale, she saw a ton of intelligent doctors come through the ranks. But this gesture, she said, should serve as a reminder that “you don’t need to be the smartest person in the room to just be there for a patient. It was pure empathic presence and human connection. It gave me hope in the next generation of physicians.”<br/><br/></p> <p> <em>A version of this article appeared on <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/how-these-young-mds-impressed-hell-out-their-bosses-2024a10007wr">Medscape.com</a></span>.</em> </p> </itemContent> </newsItem> <newsItem> <itemMeta> <itemRole>teaser</itemRole> <itemClass>text</itemClass> <title/> <deck/> </itemMeta> <itemContent> </itemContent> </newsItem> </itemSet></root>
Genetic Signatures May Predict CAR T Responders
“Our transcriptomic analysis of ZUMA-7 dataset identified novel gene expression signatures predictive of outcome with axi-cel,” the authors reported in research presented at the annual meeting of the American Association for Cancer Research earlier in April. “These gene expression signatures could support risk-stratification of LBCL patients.”
The results are from a subanalysis of the phase 3 ZUMA-7 trial in which patients with early relapsed or primary refractory LBCL were treated with axi-cel, administered as a one-time dose in the second-line setting.
Long-term results from the trial showed a 4-year overall survival of 54.6% with axi-cel versus 46.0% with the standard of care (P = .03), with a median rate of progression-free survival of 14.7 months with axi-cel versus 3.7 months in the standard-second-line treatment.
In the study, the authors noted that, “although the use of axi-cel resulted in long-term survival in more than half of treated patients, it is important to continue to strive to improve patient outcomes.”
Following up on that, senior author Simone Filosto, of Kite, a Gilead Company, of Santa Monica, California, and colleagues launched their analysis of the genetic profiles of those who did and did not have favorable responses, using data from the ZUMA-7 trial.
Using gene expression profiling with the IO-360 Nanostring gene expression panel of 769 genes, they evaluated pretreated LBCL tumor samples from 134 of the patients treated with axi-cel.
After multivariate adjustment, the results showed that those with a distinctive 6-transcript genetic expression signature, consisting of CD19, CD45RA, CCL22, KLRK1, SOX11, and SIGLEC5, had a significantly higher rate of event-free survival (hazard ratio [HR], 0.27; P = 1.82 x 10-8), as well as progression-free survival (HR, 0.27; P = 1.35 x 10-7) after treatment with axi-cel, compared with those who did not have the signature.
The authors speculated that “the 6-gene expression signature may capture lymphomas with abundant adhesion molecules, a relatively low inflammation, and abundant expression of the targeted antigen (CD19).”
Conversely, the analysis showed that increased levels of an unfavorable 17-transcript gene expression signature had a strong negative correlation with event-free survival (HR, 6.19; P = 1.51 x 10-13) and progression-free survival (HR, 7.58; P = 2.70 x 10-14).
The 17-transcript signature included CD45RO, BCL2, IL-18R1, TNFSF4 [OX40L], KLRB1 [CD161], KIR3DL2, ITGB8, DUSP5, GPC4, PSMB5, RPS6KB1, SERPINA9, NBN, GLUD1, ESR1, ARID1A, and SLC16A1.
“The 17-gene expression signature is consistent with a high level of immune infiltration and inflammation paralleled by the activation of immune-escape mechanisms, such as the upregulation of anti-apoptotic genes,” the authors explain.
Of note, the 17-gene expression signature was elevated among 18 patients who progressed after axi-cel treatment.
Importantly, the gene expression signatures were not associated with outcomes observed among patients receiving second-line standard of care in the ZUMA-7 trial. And the signatures also did not correspond with outcomes following first-line R-CHOP chemotherapy reported in two online datasets, indicating their predictive rather than prognostic value.
Commenting on the findings, Marco Ruella, MD, noted that “stratifying the [CAR T-treated] patients is extremely important given that only a subset of them, 30%-40%, will experience long-term remission.”
“In an ideal scenario, we would want to treat only the patients who would benefit from such a complex and expensive therapy,” underscored Dr. Ruella, assistant professor in the Division of Hematology/Oncology and the Center for Cellular Immunotherapies and Scientific Director of the Lymphoma Program at the Hospital of the University of Pennsylvania in Philadelphia.
A key caveat is that the results need more validation before they true gain clinical value, he noted.
“We need more data before we can use such a score in the clinic as we would need to be absolutely confident on the predictive value of such a score in additional confirmatory cohorts.”
Furthermore, caution is warranted in avoiding excluding any patients unnecessarily, he added.
“Only if there are approximately zero chances of response would we be able to exclude a patient from a treatment,” Dr. Ruella noted. “If the chance of long-term cure are minimal but still present, it might still make sense for the patient.”
Nevertheless, such findings advance the understanding of the therapy’s implication in a meaningful way, he said.
“I think this study [and similar others] are important studies that help us better understand the mechanisms of relapse,” he said.
“Translationally, we are getting closer to reaching a point where we can precisely predict outcomes and, perhaps in the future, select the patients that would benefit the most from these treatments.”
Dr. Filosto and other authors are employees of Kite, which manufactures axi-cel. Dr. Ruella treats patients with CAR T products that have been licensed to Novartis, Kite, and Vittoria Bio.
“Our transcriptomic analysis of ZUMA-7 dataset identified novel gene expression signatures predictive of outcome with axi-cel,” the authors reported in research presented at the annual meeting of the American Association for Cancer Research earlier in April. “These gene expression signatures could support risk-stratification of LBCL patients.”
The results are from a subanalysis of the phase 3 ZUMA-7 trial in which patients with early relapsed or primary refractory LBCL were treated with axi-cel, administered as a one-time dose in the second-line setting.
Long-term results from the trial showed a 4-year overall survival of 54.6% with axi-cel versus 46.0% with the standard of care (P = .03), with a median rate of progression-free survival of 14.7 months with axi-cel versus 3.7 months in the standard-second-line treatment.
In the study, the authors noted that, “although the use of axi-cel resulted in long-term survival in more than half of treated patients, it is important to continue to strive to improve patient outcomes.”
Following up on that, senior author Simone Filosto, of Kite, a Gilead Company, of Santa Monica, California, and colleagues launched their analysis of the genetic profiles of those who did and did not have favorable responses, using data from the ZUMA-7 trial.
Using gene expression profiling with the IO-360 Nanostring gene expression panel of 769 genes, they evaluated pretreated LBCL tumor samples from 134 of the patients treated with axi-cel.
After multivariate adjustment, the results showed that those with a distinctive 6-transcript genetic expression signature, consisting of CD19, CD45RA, CCL22, KLRK1, SOX11, and SIGLEC5, had a significantly higher rate of event-free survival (hazard ratio [HR], 0.27; P = 1.82 x 10-8), as well as progression-free survival (HR, 0.27; P = 1.35 x 10-7) after treatment with axi-cel, compared with those who did not have the signature.
The authors speculated that “the 6-gene expression signature may capture lymphomas with abundant adhesion molecules, a relatively low inflammation, and abundant expression of the targeted antigen (CD19).”
Conversely, the analysis showed that increased levels of an unfavorable 17-transcript gene expression signature had a strong negative correlation with event-free survival (HR, 6.19; P = 1.51 x 10-13) and progression-free survival (HR, 7.58; P = 2.70 x 10-14).
The 17-transcript signature included CD45RO, BCL2, IL-18R1, TNFSF4 [OX40L], KLRB1 [CD161], KIR3DL2, ITGB8, DUSP5, GPC4, PSMB5, RPS6KB1, SERPINA9, NBN, GLUD1, ESR1, ARID1A, and SLC16A1.
“The 17-gene expression signature is consistent with a high level of immune infiltration and inflammation paralleled by the activation of immune-escape mechanisms, such as the upregulation of anti-apoptotic genes,” the authors explain.
Of note, the 17-gene expression signature was elevated among 18 patients who progressed after axi-cel treatment.
Importantly, the gene expression signatures were not associated with outcomes observed among patients receiving second-line standard of care in the ZUMA-7 trial. And the signatures also did not correspond with outcomes following first-line R-CHOP chemotherapy reported in two online datasets, indicating their predictive rather than prognostic value.
Commenting on the findings, Marco Ruella, MD, noted that “stratifying the [CAR T-treated] patients is extremely important given that only a subset of them, 30%-40%, will experience long-term remission.”
“In an ideal scenario, we would want to treat only the patients who would benefit from such a complex and expensive therapy,” underscored Dr. Ruella, assistant professor in the Division of Hematology/Oncology and the Center for Cellular Immunotherapies and Scientific Director of the Lymphoma Program at the Hospital of the University of Pennsylvania in Philadelphia.
A key caveat is that the results need more validation before they true gain clinical value, he noted.
“We need more data before we can use such a score in the clinic as we would need to be absolutely confident on the predictive value of such a score in additional confirmatory cohorts.”
Furthermore, caution is warranted in avoiding excluding any patients unnecessarily, he added.
“Only if there are approximately zero chances of response would we be able to exclude a patient from a treatment,” Dr. Ruella noted. “If the chance of long-term cure are minimal but still present, it might still make sense for the patient.”
Nevertheless, such findings advance the understanding of the therapy’s implication in a meaningful way, he said.
“I think this study [and similar others] are important studies that help us better understand the mechanisms of relapse,” he said.
“Translationally, we are getting closer to reaching a point where we can precisely predict outcomes and, perhaps in the future, select the patients that would benefit the most from these treatments.”
Dr. Filosto and other authors are employees of Kite, which manufactures axi-cel. Dr. Ruella treats patients with CAR T products that have been licensed to Novartis, Kite, and Vittoria Bio.
“Our transcriptomic analysis of ZUMA-7 dataset identified novel gene expression signatures predictive of outcome with axi-cel,” the authors reported in research presented at the annual meeting of the American Association for Cancer Research earlier in April. “These gene expression signatures could support risk-stratification of LBCL patients.”
The results are from a subanalysis of the phase 3 ZUMA-7 trial in which patients with early relapsed or primary refractory LBCL were treated with axi-cel, administered as a one-time dose in the second-line setting.
Long-term results from the trial showed a 4-year overall survival of 54.6% with axi-cel versus 46.0% with the standard of care (P = .03), with a median rate of progression-free survival of 14.7 months with axi-cel versus 3.7 months in the standard-second-line treatment.
In the study, the authors noted that, “although the use of axi-cel resulted in long-term survival in more than half of treated patients, it is important to continue to strive to improve patient outcomes.”
Following up on that, senior author Simone Filosto, of Kite, a Gilead Company, of Santa Monica, California, and colleagues launched their analysis of the genetic profiles of those who did and did not have favorable responses, using data from the ZUMA-7 trial.
Using gene expression profiling with the IO-360 Nanostring gene expression panel of 769 genes, they evaluated pretreated LBCL tumor samples from 134 of the patients treated with axi-cel.
After multivariate adjustment, the results showed that those with a distinctive 6-transcript genetic expression signature, consisting of CD19, CD45RA, CCL22, KLRK1, SOX11, and SIGLEC5, had a significantly higher rate of event-free survival (hazard ratio [HR], 0.27; P = 1.82 x 10-8), as well as progression-free survival (HR, 0.27; P = 1.35 x 10-7) after treatment with axi-cel, compared with those who did not have the signature.
The authors speculated that “the 6-gene expression signature may capture lymphomas with abundant adhesion molecules, a relatively low inflammation, and abundant expression of the targeted antigen (CD19).”
Conversely, the analysis showed that increased levels of an unfavorable 17-transcript gene expression signature had a strong negative correlation with event-free survival (HR, 6.19; P = 1.51 x 10-13) and progression-free survival (HR, 7.58; P = 2.70 x 10-14).
The 17-transcript signature included CD45RO, BCL2, IL-18R1, TNFSF4 [OX40L], KLRB1 [CD161], KIR3DL2, ITGB8, DUSP5, GPC4, PSMB5, RPS6KB1, SERPINA9, NBN, GLUD1, ESR1, ARID1A, and SLC16A1.
“The 17-gene expression signature is consistent with a high level of immune infiltration and inflammation paralleled by the activation of immune-escape mechanisms, such as the upregulation of anti-apoptotic genes,” the authors explain.
Of note, the 17-gene expression signature was elevated among 18 patients who progressed after axi-cel treatment.
Importantly, the gene expression signatures were not associated with outcomes observed among patients receiving second-line standard of care in the ZUMA-7 trial. And the signatures also did not correspond with outcomes following first-line R-CHOP chemotherapy reported in two online datasets, indicating their predictive rather than prognostic value.
Commenting on the findings, Marco Ruella, MD, noted that “stratifying the [CAR T-treated] patients is extremely important given that only a subset of them, 30%-40%, will experience long-term remission.”
“In an ideal scenario, we would want to treat only the patients who would benefit from such a complex and expensive therapy,” underscored Dr. Ruella, assistant professor in the Division of Hematology/Oncology and the Center for Cellular Immunotherapies and Scientific Director of the Lymphoma Program at the Hospital of the University of Pennsylvania in Philadelphia.
A key caveat is that the results need more validation before they true gain clinical value, he noted.
“We need more data before we can use such a score in the clinic as we would need to be absolutely confident on the predictive value of such a score in additional confirmatory cohorts.”
Furthermore, caution is warranted in avoiding excluding any patients unnecessarily, he added.
“Only if there are approximately zero chances of response would we be able to exclude a patient from a treatment,” Dr. Ruella noted. “If the chance of long-term cure are minimal but still present, it might still make sense for the patient.”
Nevertheless, such findings advance the understanding of the therapy’s implication in a meaningful way, he said.
“I think this study [and similar others] are important studies that help us better understand the mechanisms of relapse,” he said.
“Translationally, we are getting closer to reaching a point where we can precisely predict outcomes and, perhaps in the future, select the patients that would benefit the most from these treatments.”
Dr. Filosto and other authors are employees of Kite, which manufactures axi-cel. Dr. Ruella treats patients with CAR T products that have been licensed to Novartis, Kite, and Vittoria Bio.
<!--$RCSfile: InCopy_agile.xsl,v $ $Revision: 1.35 $-->
<!--$RCSfile: drupal.xsl,v $ $Revision: 1.7 $-->
<root generator="drupal.xsl" gversion="1.7"> <header> <fileName>167836</fileName> <TBEID>0C04FC84.SIG</TBEID> <TBUniqueIdentifier>MD_0C04FC84</TBUniqueIdentifier> <newsOrJournal>News</newsOrJournal> <publisherName>Frontline Medical Communications</publisherName> <storyname>AACR_CARTGenetic</storyname> <articleType>2</articleType> <TBLocation>QC Done-All Pubs</TBLocation> <QCDate>20240424T134557</QCDate> <firstPublished>20240424T134711</firstPublished> <LastPublished>20240424T134711</LastPublished> <pubStatus qcode="stat:"/> <embargoDate/> <killDate/> <CMSDate>20240424T134711</CMSDate> <articleSource>FROM AACR 2024</articleSource> <facebookInfo/> <meetingNumber>2976-24</meetingNumber> <byline>Nancy A. Melville</byline> <bylineText>NANCY A. MELVILLE</bylineText> <bylineFull>NANCY A. MELVILLE</bylineFull> <bylineTitleText>MDedge News</bylineTitleText> <USOrGlobal/> <wireDocType/> <newsDocType/> <journalDocType/> <linkLabel/> <pageRange/> <citation/> <quizID/> <indexIssueDate/> <itemClass qcode="ninat:text"/> <provider qcode="provider:imng"> <name>IMNG Medical Media</name> <rightsInfo> <copyrightHolder> <name>Frontline Medical News</name> </copyrightHolder> <copyrightNotice>Copyright (c) 2015 Frontline Medical News, a Frontline Medical Communications Inc. company. All rights reserved. This material may not be published, broadcast, copied, or otherwise reproduced or distributed without the prior written permission of Frontline Medical Communications Inc.</copyrightNotice> </rightsInfo> </provider> <abstract/> <metaDescription>Key novel genetic signatures in patients with relapsed/refractory large B-cell lymphoma (r/r LBCL) strongly correlate with improved survival outcomes in treatme</metaDescription> <articlePDF/> <teaserImage/> <teaser>Research data suggest that key genetic clues of patients with LBCL could show which are more — or less — likely to respond to axi-cel CAR T.</teaser> <title>Genetic Signatures May Predict CAR T Responders</title> <deck/> <disclaimer/> <AuthorList/> <articleURL/> <doi/> <pubMedID/> <publishXMLStatus/> <publishXMLVersion>1</publishXMLVersion> <useEISSN>0</useEISSN> <urgency/> <pubPubdateYear/> <pubPubdateMonth/> <pubPubdateDay/> <pubVolume/> <pubNumber/> <wireChannels/> <primaryCMSID/> <CMSIDs/> <keywords/> <seeAlsos/> <publications_g> <publicationData> <publicationCode>hemn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> </publications_g> <publications> <term canonical="true">18</term> </publications> <sections> <term canonical="true">53</term> <term>39313</term> </sections> <topics> <term>61821</term> <term canonical="true">195</term> </topics> <links/> </header> <itemSet> <newsItem> <itemMeta> <itemRole>Main</itemRole> <itemClass>text</itemClass> <title>Genetic Signatures May Predict CAR T Responders</title> <deck/> </itemMeta> <itemContent> <p><span class="tag metaDescription">Key novel genetic signatures in patients with relapsed/refractory large B-cell lymphoma (r/r LBCL) strongly correlate with improved survival outcomes in treatment with the anti-CD19 CAR T-cell therapy axicabtagene ciloleucel (axi-cel).</span><br/><br/> “Our transcriptomic analysis of ZUMA-7 dataset identified novel gene expression signatures predictive of outcome with axi-cel,” the authors reported in <span class="Hyperlink"><a href="https://www.abstractsonline.com/pp8/#!/20272/presentation/10384">research presented </a></span>at the annual meeting of the American Association for Cancer Research earlier in April. “These gene expression signatures could support risk-stratification of LBCL patients.”<br/><br/>The results are from a subanalysis of the phase 3 ZUMA-7 trial in which patients with early relapsed or primary refractory LBCL were treated with axi-cel, administered as a one-time dose in the second-line setting. <br/><br/><span class="Hyperlink"><a href="ttps://www.nejm.org/doi/full/10.1056/NEJMoa2301665">Long-term results</a></span> from the trial showed a 4-year overall survival of 54.6% with axi-cel versus 46.0% with the standard of care (<em>P</em> = .03), with a median rate of progression-free survival of 14.7 months with axi-cel versus 3.7 months in the standard-second-line treatment. <br/><br/>In the study, the authors noted that, “although the use of axi-cel resulted in long-term survival in more than half of treated patients, it is important to continue to strive to improve patient outcomes.”<br/><br/>Following up on that, senior author Simone Filosto, of Kite, a Gilead Company, of Santa Monica, California, and colleagues launched their analysis of the genetic profiles of those who did and did not have favorable responses, using data from the ZUMA-7 trial.<br/><br/>Using gene expression profiling with the IO-360 Nanostring gene expression panel of 769 genes, they evaluated pretreated LBCL tumor samples from 134 of the patients treated with axi-cel. <br/><br/>After multivariate adjustment, the results showed that those with a distinctive 6-transcript genetic expression signature, consisting of CD19, CD45RA, CCL22, KLRK1, SOX11, and SIGLEC5, had a significantly higher rate of event-free survival (hazard ratio [HR], 0.27; <em>P</em> = 1.82 x 10<sup>-8</sup>), as well as progression-free survival (HR, 0.27; <em>P</em> = 1.35 x 10<sup>-7</sup>) after treatment with axi-cel, compared with those who did not have the signature. <br/><br/>The authors speculated that “the 6-gene expression signature may capture lymphomas with abundant adhesion molecules, a relatively low inflammation, and abundant expression of the targeted antigen (CD19).”<br/><br/>Conversely, the analysis showed that increased levels of an unfavorable 17-transcript gene expression signature had a strong negative correlation with event-free survival (HR, 6.19; <em>P</em> = 1.51 x 10<sup>-13</sup>) and progression-free survival (HR, 7.58; <em>P</em> = 2.70 x 10<sup>-14</sup>). <br/><br/>The 17-transcript signature included CD45RO, BCL2, IL-18R1, TNFSF4 [OX40L], KLRB1 [CD161], KIR3DL2, ITGB8, DUSP5, GPC4, PSMB5, RPS6KB1, SERPINA9, NBN, GLUD1, ESR1, ARID1A, and SLC16A1.<br/><br/>“The 17-gene expression signature is consistent with a high level of immune infiltration and inflammation paralleled by the activation of immune-escape mechanisms, such as the upregulation of anti-apoptotic genes,” the authors explain. <br/><br/>Of note, the 17-gene expression signature was elevated among 18 patients who progressed after axi-cel treatment. <br/><br/>Importantly, the gene expression signatures were not associated with outcomes observed among patients receiving second-line standard of care in the ZUMA-7 trial. And the signatures also did not correspond with outcomes following first-line R-CHOP chemotherapy reported in two online datasets, indicating their predictive rather than prognostic value.<br/><br/>Commenting on the findings, Marco Ruella, MD, noted that “stratifying the [CAR T-treated] patients is extremely important given that only a subset of them, 30%-40%, will experience long-term remission.” <br/><br/>“In an ideal scenario, we would want to treat only the patients who would benefit from such a complex and expensive therapy,” underscored Dr. Ruella, assistant professor in the Division of Hematology/Oncology and the Center for Cellular Immunotherapies and Scientific Director of the Lymphoma Program at the Hospital of the University of Pennsylvania in Philadelphia.<br/><br/>A key caveat is that the results need more validation before they true gain clinical value, he noted.<br/><br/>“We need more data before we can use such a score in the clinic as we would need to be absolutely confident on the predictive value of such a score in additional confirmatory cohorts.”<br/><br/>Furthermore, caution is warranted in avoiding excluding any patients unnecessarily, he added.<br/><br/>“Only if there are approximately zero chances of response would we be able to exclude a patient from a treatment,” Dr. Ruella noted. “If the chance of long-term cure are minimal but still present, it might still make sense for the patient.” <br/><br/>Nevertheless, such findings advance the understanding of the therapy’s implication in a meaningful way, he said. <br/><br/>“I think this study [and similar others] are important studies that help us better understand the mechanisms of relapse,” he said. <br/><br/>“Translationally, we are getting closer to reaching a point where we can precisely predict outcomes and, perhaps in the future, select the patients that would benefit the most from these treatments.”<br/><br/>Dr. Filosto and other authors are employees of Kite, which manufactures axi-cel. Dr. Ruella treats patients with CAR T products that have been licensed to Novartis, Kite, and Vittoria Bio.<span class="end"/></p> </itemContent> </newsItem> <newsItem> <itemMeta> <itemRole>teaser</itemRole> <itemClass>text</itemClass> <title/> <deck/> </itemMeta> <itemContent> </itemContent> </newsItem> </itemSet></root>
FROM AACR 2024
Federal Trade Commission Bans Noncompete Agreements, Urges More Protections for Healthcare Workers
But business groups have vowed to challenge the decision in court.
The proposed final rule passed on a 3-2 vote, with the dissenting commissioners disputing the FTC’s authority to broadly ban noncompetes.
Tensions around noncompetes have been building for years. In 2021, President Biden issued an executive order supporting measures to improve economic competition, in which he urged the FTC to consider its rulemaking authority to address noncompete clauses that unfairly limit workers’ mobility. In January 2023, per that directive, the agency proposed ending the restrictive covenants.
While the FTC estimates that the final rule will reduce healthcare costs by up to $194 billion over the next decade and increase worker earnings by $300 million annually, the ruling faces legal hurdles.
US Chamber of Commerce president and CEO Suzanne P. Clark said in a statement that the move is a “blatant power grab” that will undermine competitive business practices, adding that the Chamber will sue to block the measure.
The FTC received more than 26,000 comments on noncompetes during the public feedback period, with about 25,000 supporting the measure, said Benjamin Cady, JD, an FTC attorney.
Mr. Cady called the feedback “compelling,” citing instances of workers who were forced to commute long distances, uproot their families, or risk expensive litigation for wanting to pursue job opportunities.
For example, a comment from a physician working in Appalachia highlights the potential real-life implications of the agreements. “With hospital systems merging, providers with aggressive noncompetes must abandon the community that they serve if they [choose] to leave their employer. Healthcare providers feel trapped in their current employment situation, leading to significant burnout that can shorten their [career] longevity.”
Commissioner Alvaro Bedoya said physicians have had their lives upended by cumbersome noncompetes, often having to move out of state to practice. “A pandemic killed a million people in this country, and there are doctors who cannot work because of a noncompete,” he said.
It’s unclear whether physicians and others who work for nonprofit healthcare groups or hospitals will be covered by the new ban. FTC Commissioner Rebecca Slaughter acknowledged that the agency’s jurisdictional limitations mean that employees of “certain nonprofit organizations” may not benefit from the rule.
“We want to be transparent about the limitation and recognize there are workers, especially healthcare workers, who are bound by anticompetitive and unfair noncompete clauses, that our rule will struggle to reach,” she said. To cover nonprofit healthcare employees, Ms. Slaughter urged Congress to pass legislation banning noncompetes, such as the Workforce Mobility Act of 2021 and the Freedom to Compete Act of 2023.
The FTC final rule will take effect 120 days after it is published in the federal register, and new noncompete agreements will be banned as of this date. However, existing contracts for senior executives will remain in effect because these individuals are less likely to experience “acute harm” due to their ability to negotiate accordingly, said Mr. Cady.
States, AMA Take Aim at Noncompetes
Before the federal ban, several states had already passed legislation limiting the reach of noncompetes. According to a recent article in the Journal of the American College of Cardiology, 12 states prohibit noncompete clauses for physicians: Alabama, California, Colorado, Delaware, Massachusetts, Montana, New Hampshire, New Mexico, North Dakota, Oklahoma, Rhode Island, and South Dakota.
The remaining states allow noncompetes in some form, often excluding them for employees earning below a certain threshold. For example, in Oregon, noncompete agreements may apply to employees earning more than $113,241. Most states have provisions to adjust the threshold annually. The District of Columbia permits 2-year noncompetes for “medical specialists” earning over $250,000 annually.
Indiana employers can no longer enter into noncompete agreements with primary care providers. Other specialties may be subject to the clauses, except when the physician terminates the contract for cause or when an employer terminates the contract without cause.
Rachel Marcus, MD, a cardiologist in Washington, DC, found out how limiting her employment contract’s noncompete clause was when she wanted to leave a former position. Due to the restrictions, she told this news organization that she couldn’t work locally for a competitor for 2 years. The closest location she could seek employment without violating the agreement was Baltimore, approximately 40 miles away.
Dr. Marcus ultimately moved to another position within the same organization because of the company’s reputation for being “aggressive” in their enforcement actions.
Although the American Medical Association (AMA) does not support a total ban, its House of Delegates adopted policies last year to support the prohibition of noncompete contracts for physicians employed by for-profit or nonprofit hospitals, hospital systems, or staffing companies.
Challenges Await
The American Hospital Association, which opposed the proposed rule, called it “bad policy.” The decision “will likely be short-lived, with courts almost certain to stop it before it can do damage to hospitals’ ability to care for their patients and communities,” the association said in a statement.
To ease the transition to the new rule, the FTC also released a model language for employers to use when discussing the changes with their employees. “All employers need to do to comply with the rule is to stop enforcing existing noncompetes with workers other than senior executives and provide notice to such workers,” he said.
Dr. Marcus hopes the ban improves doctors’ lives. “Your employer is going to have to treat you better because they know that you can easily go across town to a place that has a higher salary, and your patient can go with you.”
A version of this article appeared on Medscape.com.
But business groups have vowed to challenge the decision in court.
The proposed final rule passed on a 3-2 vote, with the dissenting commissioners disputing the FTC’s authority to broadly ban noncompetes.
Tensions around noncompetes have been building for years. In 2021, President Biden issued an executive order supporting measures to improve economic competition, in which he urged the FTC to consider its rulemaking authority to address noncompete clauses that unfairly limit workers’ mobility. In January 2023, per that directive, the agency proposed ending the restrictive covenants.
While the FTC estimates that the final rule will reduce healthcare costs by up to $194 billion over the next decade and increase worker earnings by $300 million annually, the ruling faces legal hurdles.
US Chamber of Commerce president and CEO Suzanne P. Clark said in a statement that the move is a “blatant power grab” that will undermine competitive business practices, adding that the Chamber will sue to block the measure.
The FTC received more than 26,000 comments on noncompetes during the public feedback period, with about 25,000 supporting the measure, said Benjamin Cady, JD, an FTC attorney.
Mr. Cady called the feedback “compelling,” citing instances of workers who were forced to commute long distances, uproot their families, or risk expensive litigation for wanting to pursue job opportunities.
For example, a comment from a physician working in Appalachia highlights the potential real-life implications of the agreements. “With hospital systems merging, providers with aggressive noncompetes must abandon the community that they serve if they [choose] to leave their employer. Healthcare providers feel trapped in their current employment situation, leading to significant burnout that can shorten their [career] longevity.”
Commissioner Alvaro Bedoya said physicians have had their lives upended by cumbersome noncompetes, often having to move out of state to practice. “A pandemic killed a million people in this country, and there are doctors who cannot work because of a noncompete,” he said.
It’s unclear whether physicians and others who work for nonprofit healthcare groups or hospitals will be covered by the new ban. FTC Commissioner Rebecca Slaughter acknowledged that the agency’s jurisdictional limitations mean that employees of “certain nonprofit organizations” may not benefit from the rule.
“We want to be transparent about the limitation and recognize there are workers, especially healthcare workers, who are bound by anticompetitive and unfair noncompete clauses, that our rule will struggle to reach,” she said. To cover nonprofit healthcare employees, Ms. Slaughter urged Congress to pass legislation banning noncompetes, such as the Workforce Mobility Act of 2021 and the Freedom to Compete Act of 2023.
The FTC final rule will take effect 120 days after it is published in the federal register, and new noncompete agreements will be banned as of this date. However, existing contracts for senior executives will remain in effect because these individuals are less likely to experience “acute harm” due to their ability to negotiate accordingly, said Mr. Cady.
States, AMA Take Aim at Noncompetes
Before the federal ban, several states had already passed legislation limiting the reach of noncompetes. According to a recent article in the Journal of the American College of Cardiology, 12 states prohibit noncompete clauses for physicians: Alabama, California, Colorado, Delaware, Massachusetts, Montana, New Hampshire, New Mexico, North Dakota, Oklahoma, Rhode Island, and South Dakota.
The remaining states allow noncompetes in some form, often excluding them for employees earning below a certain threshold. For example, in Oregon, noncompete agreements may apply to employees earning more than $113,241. Most states have provisions to adjust the threshold annually. The District of Columbia permits 2-year noncompetes for “medical specialists” earning over $250,000 annually.
Indiana employers can no longer enter into noncompete agreements with primary care providers. Other specialties may be subject to the clauses, except when the physician terminates the contract for cause or when an employer terminates the contract without cause.
Rachel Marcus, MD, a cardiologist in Washington, DC, found out how limiting her employment contract’s noncompete clause was when she wanted to leave a former position. Due to the restrictions, she told this news organization that she couldn’t work locally for a competitor for 2 years. The closest location she could seek employment without violating the agreement was Baltimore, approximately 40 miles away.
Dr. Marcus ultimately moved to another position within the same organization because of the company’s reputation for being “aggressive” in their enforcement actions.
Although the American Medical Association (AMA) does not support a total ban, its House of Delegates adopted policies last year to support the prohibition of noncompete contracts for physicians employed by for-profit or nonprofit hospitals, hospital systems, or staffing companies.
Challenges Await
The American Hospital Association, which opposed the proposed rule, called it “bad policy.” The decision “will likely be short-lived, with courts almost certain to stop it before it can do damage to hospitals’ ability to care for their patients and communities,” the association said in a statement.
To ease the transition to the new rule, the FTC also released a model language for employers to use when discussing the changes with their employees. “All employers need to do to comply with the rule is to stop enforcing existing noncompetes with workers other than senior executives and provide notice to such workers,” he said.
Dr. Marcus hopes the ban improves doctors’ lives. “Your employer is going to have to treat you better because they know that you can easily go across town to a place that has a higher salary, and your patient can go with you.”
A version of this article appeared on Medscape.com.
But business groups have vowed to challenge the decision in court.
The proposed final rule passed on a 3-2 vote, with the dissenting commissioners disputing the FTC’s authority to broadly ban noncompetes.
Tensions around noncompetes have been building for years. In 2021, President Biden issued an executive order supporting measures to improve economic competition, in which he urged the FTC to consider its rulemaking authority to address noncompete clauses that unfairly limit workers’ mobility. In January 2023, per that directive, the agency proposed ending the restrictive covenants.
While the FTC estimates that the final rule will reduce healthcare costs by up to $194 billion over the next decade and increase worker earnings by $300 million annually, the ruling faces legal hurdles.
US Chamber of Commerce president and CEO Suzanne P. Clark said in a statement that the move is a “blatant power grab” that will undermine competitive business practices, adding that the Chamber will sue to block the measure.
The FTC received more than 26,000 comments on noncompetes during the public feedback period, with about 25,000 supporting the measure, said Benjamin Cady, JD, an FTC attorney.
Mr. Cady called the feedback “compelling,” citing instances of workers who were forced to commute long distances, uproot their families, or risk expensive litigation for wanting to pursue job opportunities.
For example, a comment from a physician working in Appalachia highlights the potential real-life implications of the agreements. “With hospital systems merging, providers with aggressive noncompetes must abandon the community that they serve if they [choose] to leave their employer. Healthcare providers feel trapped in their current employment situation, leading to significant burnout that can shorten their [career] longevity.”
Commissioner Alvaro Bedoya said physicians have had their lives upended by cumbersome noncompetes, often having to move out of state to practice. “A pandemic killed a million people in this country, and there are doctors who cannot work because of a noncompete,” he said.
It’s unclear whether physicians and others who work for nonprofit healthcare groups or hospitals will be covered by the new ban. FTC Commissioner Rebecca Slaughter acknowledged that the agency’s jurisdictional limitations mean that employees of “certain nonprofit organizations” may not benefit from the rule.
“We want to be transparent about the limitation and recognize there are workers, especially healthcare workers, who are bound by anticompetitive and unfair noncompete clauses, that our rule will struggle to reach,” she said. To cover nonprofit healthcare employees, Ms. Slaughter urged Congress to pass legislation banning noncompetes, such as the Workforce Mobility Act of 2021 and the Freedom to Compete Act of 2023.
The FTC final rule will take effect 120 days after it is published in the federal register, and new noncompete agreements will be banned as of this date. However, existing contracts for senior executives will remain in effect because these individuals are less likely to experience “acute harm” due to their ability to negotiate accordingly, said Mr. Cady.
States, AMA Take Aim at Noncompetes
Before the federal ban, several states had already passed legislation limiting the reach of noncompetes. According to a recent article in the Journal of the American College of Cardiology, 12 states prohibit noncompete clauses for physicians: Alabama, California, Colorado, Delaware, Massachusetts, Montana, New Hampshire, New Mexico, North Dakota, Oklahoma, Rhode Island, and South Dakota.
The remaining states allow noncompetes in some form, often excluding them for employees earning below a certain threshold. For example, in Oregon, noncompete agreements may apply to employees earning more than $113,241. Most states have provisions to adjust the threshold annually. The District of Columbia permits 2-year noncompetes for “medical specialists” earning over $250,000 annually.
Indiana employers can no longer enter into noncompete agreements with primary care providers. Other specialties may be subject to the clauses, except when the physician terminates the contract for cause or when an employer terminates the contract without cause.
Rachel Marcus, MD, a cardiologist in Washington, DC, found out how limiting her employment contract’s noncompete clause was when she wanted to leave a former position. Due to the restrictions, she told this news organization that she couldn’t work locally for a competitor for 2 years. The closest location she could seek employment without violating the agreement was Baltimore, approximately 40 miles away.
Dr. Marcus ultimately moved to another position within the same organization because of the company’s reputation for being “aggressive” in their enforcement actions.
Although the American Medical Association (AMA) does not support a total ban, its House of Delegates adopted policies last year to support the prohibition of noncompete contracts for physicians employed by for-profit or nonprofit hospitals, hospital systems, or staffing companies.
Challenges Await
The American Hospital Association, which opposed the proposed rule, called it “bad policy.” The decision “will likely be short-lived, with courts almost certain to stop it before it can do damage to hospitals’ ability to care for their patients and communities,” the association said in a statement.
To ease the transition to the new rule, the FTC also released a model language for employers to use when discussing the changes with their employees. “All employers need to do to comply with the rule is to stop enforcing existing noncompetes with workers other than senior executives and provide notice to such workers,” he said.
Dr. Marcus hopes the ban improves doctors’ lives. “Your employer is going to have to treat you better because they know that you can easily go across town to a place that has a higher salary, and your patient can go with you.”
A version of this article appeared on Medscape.com.
<!--$RCSfile: InCopy_agile.xsl,v $ $Revision: 1.35 $-->
<!--$RCSfile: drupal.xsl,v $ $Revision: 1.7 $-->
<root generator="drupal.xsl" gversion="1.7"> <header> <fileName>167842</fileName> <TBEID>0C04FC9A.SIG</TBEID> <TBUniqueIdentifier>MD_0C04FC9A</TBUniqueIdentifier> <newsOrJournal>News</newsOrJournal> <publisherName>Frontline Medical Communications</publisherName> <storyname/> <articleType>2</articleType> <TBLocation>QC Done-All Pubs</TBLocation> <QCDate>20240424T122750</QCDate> <firstPublished>20240424T122826</firstPublished> <LastPublished>20240424T122826</LastPublished> <pubStatus qcode="stat:"/> <embargoDate/> <killDate/> <CMSDate>20240424T122826</CMSDate> <articleSource/> <facebookInfo/> <meetingNumber/> <byline>Steph Weber</byline> <bylineText>STEPH WEBER</bylineText> <bylineFull>STEPH WEBER</bylineFull> <bylineTitleText/> <USOrGlobal/> <wireDocType/> <newsDocType>Feature</newsDocType> <journalDocType/> <linkLabel/> <pageRange/> <citation/> <quizID/> <indexIssueDate/> <itemClass qcode="ninat:text"/> <provider qcode="provider:imng"> <name>IMNG Medical Media</name> <rightsInfo> <copyrightHolder> <name>Frontline Medical News</name> </copyrightHolder> <copyrightNotice>Copyright (c) 2015 Frontline Medical News, a Frontline Medical Communications Inc. company. All rights reserved. This material may not be published, broadcast, copied, or otherwise reproduced or distributed without the prior written permission of Frontline Medical Communications Inc.</copyrightNotice> </rightsInfo> </provider> <abstract/> <metaDescription>The Federal Trade Commission (FTC) voted Tuesday to ban noncompete agreements, possibly making it easier for doctors to switch employers without having to leave</metaDescription> <articlePDF/> <teaserImage/> <teaser>But dissenting commissioners dispute the FTC’s authority to broadly ban noncompetes.</teaser> <title>Federal Trade Commission Bans Noncompete Agreements, Urges More Protections for Healthcare Workers</title> <deck/> <disclaimer/> <AuthorList/> <articleURL/> <doi/> <pubMedID/> <publishXMLStatus/> <publishXMLVersion>1</publishXMLVersion> <useEISSN>0</useEISSN> <urgency/> <pubPubdateYear/> <pubPubdateMonth/> <pubPubdateDay/> <pubVolume/> <pubNumber/> <wireChannels/> <primaryCMSID/> <CMSIDs/> <keywords/> <seeAlsos/> <publications_g> <publicationData> <publicationCode>card</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>endo</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>chph</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>cpn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>skin</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>fp</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>hemn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>idprac</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>im</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>rn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>oncr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>ob</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>pn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>nr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle>Neurology Reviews</journalTitle> <journalFullTitle>Neurology Reviews</journalFullTitle> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>mdsurg</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>icymicov</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>mdemed</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement/> </publicationData> <publicationData> <publicationCode>mdid</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>GIHOLD</publicationCode> <pubIssueName>January 2014</pubIssueName> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement/> </publicationData> </publications_g> <publications> <term>5</term> <term>34</term> <term>6</term> <term>9</term> <term>13</term> <term canonical="true">15</term> <term>18</term> <term>20</term> <term>21</term> <term>26</term> <term>31</term> <term>23</term> <term>25</term> <term>22</term> <term>52226</term> <term>69586</term> <term>58877</term> <term>51892</term> </publications> <sections> <term canonical="true">27980</term> <term>39313</term> <term>26933</term> </sections> <topics> <term canonical="true">38029</term> <term>278</term> <term>50194</term> <term>63993</term> </topics> <links/> </header> <itemSet> <newsItem> <itemMeta> <itemRole>Main</itemRole> <itemClass>text</itemClass> <title>Federal Trade Commission Bans Noncompete Agreements, Urges More Protections for Healthcare Workers</title> <deck/> </itemMeta> <itemContent> <p><span class="tag metaDescription">The Federal Trade Commission (FTC) voted Tuesday to ban noncompete agreements, possibly making it easier for doctors to switch employers without having to leave their communities and patients behind.</span> But business groups have vowed to challenge the decision in court.</p> <p>The <span class="Hyperlink"><a href="https://www.ftc.gov/news-events/news/press-releases/2024/04/ftc-announces-rule-banning-noncompetes">proposed final rule</a></span> passed on a 3-2 vote, with the dissenting commissioners disputing the FTC’s authority to broadly ban noncompetes.<br/><br/>Tensions around noncompetes have been building for years. In 2021, President Biden issued an <span class="Hyperlink"><a href="https://www.whitehouse.gov/briefing-room/presidential-actions/2021/07/09/executive-order-on-promoting-competition-in-the-american-economy/">executive order</a></span> supporting measures to improve economic competition, in which he urged the FTC to consider its rulemaking authority to address noncompete clauses that unfairly limit workers’ mobility. In January 2023, per that directive, the agency <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/986904">proposed ending the restrictive covenants</a></span>.<br/><br/>While the FTC estimates that the final rule will reduce healthcare costs by up to $194 billion over the next decade and increase worker earnings by $300 million annually, the ruling faces legal hurdles.<br/><br/>US Chamber of Commerce president and CEO Suzanne P. Clark said in a <span class="Hyperlink"><a href="https://www.uschamber.com/finance/antitrust/u-s-chamber-to-sue-ftc-over-unlawful-power-grab-on-noncompete-agreements-ban">statement</a></span> that the move is a “blatant power grab” that will undermine competitive business practices, adding that the Chamber will sue to block the measure.<br/><br/>The FTC received more than 26,000 comments on noncompetes during the public feedback period, with about 25,000 supporting the measure, said Benjamin Cady, JD, an FTC attorney.<br/><br/>Mr. Cady called the feedback “compelling,” citing instances of workers who were forced to commute long distances, uproot their families, or <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/urologist-sues-health-system-over-noncompete-clause-2024a1000389">risk expensive litigation</a></span> for wanting to pursue job opportunities.<br/><br/>For example, a comment from a physician working in Appalachia highlights the potential real-life implications of the agreements. “With <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/hospital-mergers-2024-five-things-know-2024a100047m">hospital systems merging</a></span>, providers with aggressive noncompetes must abandon the community that they serve if they [choose] to leave their employer. Healthcare providers feel trapped in their current employment situation, leading to <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/some-mds-long-covid-burnout-new-reality-2024a10006hq">significant burnout</a></span> that can shorten their [career] longevity.”<br/><br/>Commissioner Alvaro Bedoya said physicians have had their <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/989694">lives upended</a></span> by cumbersome noncompetes, often having to move out of state to practice. “A pandemic killed a million people in this country, and there are doctors who cannot work because of a noncompete,” he said.<br/><br/>It’s unclear whether physicians and others who work for nonprofit healthcare groups or hospitals will be covered by the new ban. FTC Commissioner Rebecca Slaughter acknowledged that the agency’s jurisdictional limitations mean that employees of “certain nonprofit organizations” may not benefit from the rule.<br/><br/>“We want to be transparent about the limitation and recognize there are workers, especially healthcare workers, who are bound by anticompetitive and unfair noncompete clauses, that our rule will struggle to reach,” she said. To cover nonprofit healthcare employees, Ms. Slaughter urged Congress to pass legislation banning noncompetes, such as the <span class="Hyperlink"><a href="https://www.congress.gov/bill/117th-congress/senate-bill/483">Workforce Mobility Act of 2021</a></span> and the <span class="Hyperlink"><a href="https://www.congress.gov/bill/118th-congress/senate-bill/379">Freedom to Compete Act of 2023</a></span>.<br/><br/>The FTC final rule will take effect 120 days after it is published in the federal register, and new noncompete agreements will be banned as of this date. However, existing contracts for senior executives will remain in effect because these individuals are less likely to experience “acute harm” due to their ability to negotiate accordingly, said Mr. Cady.<br/><br/></p> <h2>States, AMA Take Aim at Noncompetes</h2> <p>Before the federal ban, several states had already passed legislation limiting the reach of noncompetes. According to a recent article in the <em>Journal of the American College of Cardiology</em>, <span class="Hyperlink"><a href="https://www.jacc.org/doi/10.1016/j.jacadv.2023.100547">12 states</a></span> prohibit noncompete clauses for physicians: Alabama, California, Colorado, Delaware, Massachusetts, Montana, New Hampshire, New Mexico, North Dakota, Oklahoma, Rhode Island, and South Dakota.<br/><br/>The remaining states allow noncompetes in some form, often excluding them for employees earning below a certain threshold. For example, in <span class="Hyperlink"><a href="https://www.oregon.gov/boli/employers/pages/noncompetition-agreements.aspx">Oregon</a></span>, noncompete agreements may apply to employees earning more than $113,241. Most states have provisions to adjust the threshold annually. The District of Columbia permits <span class="Hyperlink"><a href="https://oag.dc.gov/blog/worker-alert-noncompete-provisions-are-now-illegal">2-year noncompetes</a></span> for “medical specialists” earning over $250,000 annually.<br/><br/>Indiana employers can no longer enter into noncompete agreements with <span class="Hyperlink"><a href="https://iga.in.gov/legislative/2023/bills/senate/7/details">primary care providers</a></span>. Other specialties may be subject to the clauses, except when the physician <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/994478">terminates the contract for cause</a></span> or when an employer terminates the contract without cause.<br/><br/>Rachel Marcus, MD, a cardiologist in Washington, DC, found out how limiting her employment contract’s noncompete clause was when she wanted to leave a former position. Due to the restrictions, she told this news organization that she couldn’t work locally for a competitor for 2 years. The closest location she could seek employment without violating the agreement was Baltimore, approximately 40 miles away.<br/><br/>Dr. Marcus ultimately moved to another position within the same organization because of the company’s reputation for being “aggressive” in their enforcement actions.<br/><br/>Although the American Medical Association (AMA) does not support a total ban, its House of Delegates <span class="Hyperlink"><a href="https://www.ama-assn.org/medical-residents/transition-resident-attending/ama-backs-effort-ban-many-physician-noncompete">adopted policies</a></span> last year to support the prohibition of noncompete contracts for physicians employed by for-profit or nonprofit hospitals, hospital systems, or staffing companies.<br/><br/></p> <h2>Challenges Await</h2> <p>The American Hospital Association, which opposed the proposed rule, called it “bad policy.” The decision “will likely be short-lived, with courts almost certain to stop it before it can do damage to hospitals’ ability to care for their patients and communities,” the association said in a <span class="Hyperlink"><a href="https://www.aha.org/press-releases/2024-04-23-aha-statement-final-ftc-noncompete-regulation">statement</a></span>.<br/><br/>To ease the transition to the new rule, the FTC also released a <span class="Hyperlink"><a href="https://www.ftc.gov/legal-library/browse/rules/noncompete-rule">model language</a></span> for employers to use when discussing the changes with their employees. “All employers need to do to comply with the rule is to stop enforcing existing noncompetes with workers other than senior executives and provide notice to such workers,” he said.<br/><br/>Dr. Marcus hopes the ban <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/are-you-ready-ai-be-better-doctor-than-you-2024a100070q">improves doctors’ lives</a></span>. “Your employer is going to have to treat you better because they know that you can easily go across town to a place that has a higher salary, and your patient can go with you.”<span class="end"/></p> <p> <em>A version of this article appeared on <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/federal-trade-commission-bans-noncompete-agreements-urges-2024a10007y0">Medscape.com</a></span>.</em> </p> </itemContent> </newsItem> <newsItem> <itemMeta> <itemRole>teaser</itemRole> <itemClass>text</itemClass> <title/> <deck/> </itemMeta> <itemContent> </itemContent> </newsItem> </itemSet></root>
Are Women Better Doctors Than Men?
This transcript has been edited for clarity.
It’s a battle of the sexes today as we dive into a paper that makes you say, “Wow, what an interesting study” and also “Boy, am I glad I didn’t do that study.” That’s because studies like this are always somewhat fraught; they say something about medicine but also something about society — and that makes this a bit precarious. But that’s never stopped us before. So, let’s go ahead and try to answer the question: Do women make better doctors than men?
On the surface, this question seems nearly impossible to answer. It’s too broad; what does it mean to be a “better” doctor? At first blush it seems that there are just too many variables to control for here: the type of doctor, the type of patient, the clinical scenario, and so on.
But this study, “Comparison of hospital mortality and readmission rates by physician and patient sex,” which appears in Annals of Internal Medicine, uses a fairly ingenious method to cut through all the bias by leveraging two simple facts: First, hospital medicine is largely conducted by hospitalists these days; second, due to the shift-based nature of hospitalist work, the hospitalist you get when you are admitted to the hospital is pretty much random.
In other words, if you are admitted to the hospital for an acute illness and get a hospitalist as your attending, you have no control over whether it is a man or a woman. Is this a randomized trial? No, but it’s not bad.
Researchers used Medicare claims data to identify adults over age 65 who had nonelective hospital admissions throughout the United States. The claims revealed the sex of the patient and the name of the attending physician. By linking to a medical provider database, they could determine the sex of the provider.
The goal was to look at outcomes across four dyads:
- Male patient – male doctor
- Male patient – female doctor
- Female patient – male doctor
- Female patient – female doctor
The primary outcome was 30-day mortality.
I told you that focusing on hospitalists produces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by approximately 50,000 physicians, 30% of whom were female. And, though female patients and male patients differed, they did not differ with respect to the sex of their hospitalist. So, by physician sex, patients were similar in mean age, race, ethnicity, household income, eligibility for Medicaid, and comorbid conditions. The authors even created a “predicted mortality” score which was similar across the groups as well.
Now, the female physicians were a bit different from the male physicians. The female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year, and were a bit younger.
So, we have broadly similar patients regardless of who their hospitalist was, but hospitalists differ by factors other than their sex. Fine.
I’ve graphed the results here. 
This is a relatively small effect, to be sure, but if you multiply it across the millions of hospitalist admissions per year, you can start to put up some real numbers.
So, what is going on here? I see four broad buckets of possibilities.
Let’s start with the obvious explanation: Women, on average, are better doctors than men. I am married to a woman doctor, and based on my personal experience, this explanation is undoubtedly true. But why would that be?
The authors cite data that suggest that female physicians are less likely than male physicians to dismiss patient concerns — and in particular, the concerns of female patients — perhaps leading to fewer missed diagnoses. But this is impossible to measure with administrative data, so this study can no more tell us whether these female hospitalists are more attentive than their male counterparts than it can suggest that the benefit is mediated by the shorter average height of female physicians. Perhaps the key is being closer to the patient?
The second possibility here is that this has nothing to do with the sex of the physician at all; it has to do with those other things that associate with the sex of the physician. We know, for example, that the female physicians saw fewer patients per year than the male physicians, but the study authors adjusted for this in the statistical models. Still, other unmeasured factors (confounders) could be present. By the way, confounders wouldn’t necessarily change the primary finding — you are better off being cared for by female physicians. It’s just not because they are female; it’s a convenient marker for some other quality, such as age.
The third possibility is that the study represents a phenomenon called collider bias. The idea here is that physicians only get into the study if they are hospitalists, and the quality of physicians who choose to become a hospitalist may differ by sex. When deciding on a specialty, a talented resident considering certain lifestyle issues may find hospital medicine particularly attractive — and that draw toward a more lifestyle-friendly specialty may differ by sex, as some prior studies have shown. If true, the pool of women hospitalists may be better than their male counterparts because male physicians of that caliber don’t become hospitalists.
Okay, don’t write in. I’m just trying to cite examples of how to think about collider bias. I can’t prove that this is the case, and in fact the authors do a sensitivity analysis of all physicians, not just hospitalists, and show the same thing. So this is probably not true, but epidemiology is fun, right?
And the fourth possibility: This is nothing but statistical noise. The effect size is incredibly small and just on the border of statistical significance. Especially when you’re working with very large datasets like this, you’ve got to be really careful about overinterpreting statistically significant findings that are nevertheless of small magnitude.
Regardless, it’s an interesting study, one that made me think and, of course, worry a bit about how I would present it. Forgive me if I’ve been indelicate in handling the complex issues of sex, gender, and society here. But I’m not sure what you expect; after all, I’m only a male doctor.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s a battle of the sexes today as we dive into a paper that makes you say, “Wow, what an interesting study” and also “Boy, am I glad I didn’t do that study.” That’s because studies like this are always somewhat fraught; they say something about medicine but also something about society — and that makes this a bit precarious. But that’s never stopped us before. So, let’s go ahead and try to answer the question: Do women make better doctors than men?
On the surface, this question seems nearly impossible to answer. It’s too broad; what does it mean to be a “better” doctor? At first blush it seems that there are just too many variables to control for here: the type of doctor, the type of patient, the clinical scenario, and so on.
But this study, “Comparison of hospital mortality and readmission rates by physician and patient sex,” which appears in Annals of Internal Medicine, uses a fairly ingenious method to cut through all the bias by leveraging two simple facts: First, hospital medicine is largely conducted by hospitalists these days; second, due to the shift-based nature of hospitalist work, the hospitalist you get when you are admitted to the hospital is pretty much random.
In other words, if you are admitted to the hospital for an acute illness and get a hospitalist as your attending, you have no control over whether it is a man or a woman. Is this a randomized trial? No, but it’s not bad.
Researchers used Medicare claims data to identify adults over age 65 who had nonelective hospital admissions throughout the United States. The claims revealed the sex of the patient and the name of the attending physician. By linking to a medical provider database, they could determine the sex of the provider.
The goal was to look at outcomes across four dyads:
- Male patient – male doctor
- Male patient – female doctor
- Female patient – male doctor
- Female patient – female doctor
The primary outcome was 30-day mortality.
I told you that focusing on hospitalists produces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by approximately 50,000 physicians, 30% of whom were female. And, though female patients and male patients differed, they did not differ with respect to the sex of their hospitalist. So, by physician sex, patients were similar in mean age, race, ethnicity, household income, eligibility for Medicaid, and comorbid conditions. The authors even created a “predicted mortality” score which was similar across the groups as well.
Now, the female physicians were a bit different from the male physicians. The female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year, and were a bit younger.
So, we have broadly similar patients regardless of who their hospitalist was, but hospitalists differ by factors other than their sex. Fine.
I’ve graphed the results here. 
This is a relatively small effect, to be sure, but if you multiply it across the millions of hospitalist admissions per year, you can start to put up some real numbers.
So, what is going on here? I see four broad buckets of possibilities.
Let’s start with the obvious explanation: Women, on average, are better doctors than men. I am married to a woman doctor, and based on my personal experience, this explanation is undoubtedly true. But why would that be?
The authors cite data that suggest that female physicians are less likely than male physicians to dismiss patient concerns — and in particular, the concerns of female patients — perhaps leading to fewer missed diagnoses. But this is impossible to measure with administrative data, so this study can no more tell us whether these female hospitalists are more attentive than their male counterparts than it can suggest that the benefit is mediated by the shorter average height of female physicians. Perhaps the key is being closer to the patient?
The second possibility here is that this has nothing to do with the sex of the physician at all; it has to do with those other things that associate with the sex of the physician. We know, for example, that the female physicians saw fewer patients per year than the male physicians, but the study authors adjusted for this in the statistical models. Still, other unmeasured factors (confounders) could be present. By the way, confounders wouldn’t necessarily change the primary finding — you are better off being cared for by female physicians. It’s just not because they are female; it’s a convenient marker for some other quality, such as age.
The third possibility is that the study represents a phenomenon called collider bias. The idea here is that physicians only get into the study if they are hospitalists, and the quality of physicians who choose to become a hospitalist may differ by sex. When deciding on a specialty, a talented resident considering certain lifestyle issues may find hospital medicine particularly attractive — and that draw toward a more lifestyle-friendly specialty may differ by sex, as some prior studies have shown. If true, the pool of women hospitalists may be better than their male counterparts because male physicians of that caliber don’t become hospitalists.
Okay, don’t write in. I’m just trying to cite examples of how to think about collider bias. I can’t prove that this is the case, and in fact the authors do a sensitivity analysis of all physicians, not just hospitalists, and show the same thing. So this is probably not true, but epidemiology is fun, right?
And the fourth possibility: This is nothing but statistical noise. The effect size is incredibly small and just on the border of statistical significance. Especially when you’re working with very large datasets like this, you’ve got to be really careful about overinterpreting statistically significant findings that are nevertheless of small magnitude.
Regardless, it’s an interesting study, one that made me think and, of course, worry a bit about how I would present it. Forgive me if I’ve been indelicate in handling the complex issues of sex, gender, and society here. But I’m not sure what you expect; after all, I’m only a male doctor.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
It’s a battle of the sexes today as we dive into a paper that makes you say, “Wow, what an interesting study” and also “Boy, am I glad I didn’t do that study.” That’s because studies like this are always somewhat fraught; they say something about medicine but also something about society — and that makes this a bit precarious. But that’s never stopped us before. So, let’s go ahead and try to answer the question: Do women make better doctors than men?
On the surface, this question seems nearly impossible to answer. It’s too broad; what does it mean to be a “better” doctor? At first blush it seems that there are just too many variables to control for here: the type of doctor, the type of patient, the clinical scenario, and so on.
But this study, “Comparison of hospital mortality and readmission rates by physician and patient sex,” which appears in Annals of Internal Medicine, uses a fairly ingenious method to cut through all the bias by leveraging two simple facts: First, hospital medicine is largely conducted by hospitalists these days; second, due to the shift-based nature of hospitalist work, the hospitalist you get when you are admitted to the hospital is pretty much random.
In other words, if you are admitted to the hospital for an acute illness and get a hospitalist as your attending, you have no control over whether it is a man or a woman. Is this a randomized trial? No, but it’s not bad.
Researchers used Medicare claims data to identify adults over age 65 who had nonelective hospital admissions throughout the United States. The claims revealed the sex of the patient and the name of the attending physician. By linking to a medical provider database, they could determine the sex of the provider.
The goal was to look at outcomes across four dyads:
- Male patient – male doctor
- Male patient – female doctor
- Female patient – male doctor
- Female patient – female doctor
The primary outcome was 30-day mortality.
I told you that focusing on hospitalists produces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by approximately 50,000 physicians, 30% of whom were female. And, though female patients and male patients differed, they did not differ with respect to the sex of their hospitalist. So, by physician sex, patients were similar in mean age, race, ethnicity, household income, eligibility for Medicaid, and comorbid conditions. The authors even created a “predicted mortality” score which was similar across the groups as well.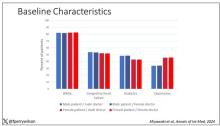
Now, the female physicians were a bit different from the male physicians. The female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year, and were a bit younger.
So, we have broadly similar patients regardless of who their hospitalist was, but hospitalists differ by factors other than their sex. Fine.
I’ve graphed the results here. 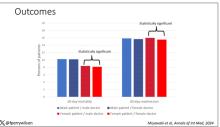
This is a relatively small effect, to be sure, but if you multiply it across the millions of hospitalist admissions per year, you can start to put up some real numbers.
So, what is going on here? I see four broad buckets of possibilities.
Let’s start with the obvious explanation: Women, on average, are better doctors than men. I am married to a woman doctor, and based on my personal experience, this explanation is undoubtedly true. But why would that be?
The authors cite data that suggest that female physicians are less likely than male physicians to dismiss patient concerns — and in particular, the concerns of female patients — perhaps leading to fewer missed diagnoses. But this is impossible to measure with administrative data, so this study can no more tell us whether these female hospitalists are more attentive than their male counterparts than it can suggest that the benefit is mediated by the shorter average height of female physicians. Perhaps the key is being closer to the patient?
The second possibility here is that this has nothing to do with the sex of the physician at all; it has to do with those other things that associate with the sex of the physician. We know, for example, that the female physicians saw fewer patients per year than the male physicians, but the study authors adjusted for this in the statistical models. Still, other unmeasured factors (confounders) could be present. By the way, confounders wouldn’t necessarily change the primary finding — you are better off being cared for by female physicians. It’s just not because they are female; it’s a convenient marker for some other quality, such as age.
The third possibility is that the study represents a phenomenon called collider bias. The idea here is that physicians only get into the study if they are hospitalists, and the quality of physicians who choose to become a hospitalist may differ by sex. When deciding on a specialty, a talented resident considering certain lifestyle issues may find hospital medicine particularly attractive — and that draw toward a more lifestyle-friendly specialty may differ by sex, as some prior studies have shown. If true, the pool of women hospitalists may be better than their male counterparts because male physicians of that caliber don’t become hospitalists.
Okay, don’t write in. I’m just trying to cite examples of how to think about collider bias. I can’t prove that this is the case, and in fact the authors do a sensitivity analysis of all physicians, not just hospitalists, and show the same thing. So this is probably not true, but epidemiology is fun, right?
And the fourth possibility: This is nothing but statistical noise. The effect size is incredibly small and just on the border of statistical significance. Especially when you’re working with very large datasets like this, you’ve got to be really careful about overinterpreting statistically significant findings that are nevertheless of small magnitude.
Regardless, it’s an interesting study, one that made me think and, of course, worry a bit about how I would present it. Forgive me if I’ve been indelicate in handling the complex issues of sex, gender, and society here. But I’m not sure what you expect; after all, I’m only a male doctor.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
<!--$RCSfile: InCopy_agile.xsl,v $ $Revision: 1.35 $-->
<!--$RCSfile: drupal.xsl,v $ $Revision: 1.7 $-->
<root generator="drupal.xsl" gversion="1.7"> <header> <fileName>167829</fileName> <TBEID>0C04FC71.SIG</TBEID> <TBUniqueIdentifier>MD_0C04FC71</TBUniqueIdentifier> <newsOrJournal>News</newsOrJournal> <publisherName>Frontline Medical Communications</publisherName> <storyname/> <articleType>2</articleType> <TBLocation>QC Done-All Pubs</TBLocation> <QCDate>20240424T111623</QCDate> <firstPublished>20240424T113542</firstPublished> <LastPublished>20240424T113542</LastPublished> <pubStatus qcode="stat:"/> <embargoDate/> <killDate/> <CMSDate>20240424T113541</CMSDate> <articleSource/> <facebookInfo/> <meetingNumber/> <byline>F. Perry Wilson, MD</byline> <bylineText>F. PERRY WILSON, MD, MSCE</bylineText> <bylineFull>F. PERRY WILSON, MD, MSCE</bylineFull> <bylineTitleText/> <USOrGlobal/> <wireDocType/> <newsDocType>News</newsDocType> <journalDocType/> <linkLabel/> <pageRange/> <citation/> <quizID/> <indexIssueDate/> <itemClass qcode="ninat:text"/> <provider qcode="provider:imng"> <name>IMNG Medical Media</name> <rightsInfo> <copyrightHolder> <name>Frontline Medical News</name> </copyrightHolder> <copyrightNotice>Copyright (c) 2015 Frontline Medical News, a Frontline Medical Communications Inc. company. All rights reserved. This material may not be published, broadcast, copied, or otherwise reproduced or distributed without the prior written permission of Frontline Medical Communications Inc.</copyrightNotice> </rightsInfo> </provider> <abstract/> <metaDescription>Female patients had a significantly lower 30-day mortality rate than male patients, but they fared even better when cared for by female doctors compared with ma</metaDescription> <articlePDF/> <teaserImage>301165</teaserImage> <teaser>Study finds female hospitalists provided better care, defined as lower 30-day mortality, than male hospitalists.</teaser> <title>Are Women Better Doctors Than Men?</title> <deck/> <disclaimer/> <AuthorList/> <articleURL/> <doi/> <pubMedID/> <publishXMLStatus/> <publishXMLVersion>1</publishXMLVersion> <useEISSN>0</useEISSN> <urgency/> <pubPubdateYear/> <pubPubdateMonth/> <pubPubdateDay/> <pubVolume/> <pubNumber/> <wireChannels/> <primaryCMSID/> <CMSIDs/> <keywords/> <seeAlsos/> <publications_g> <publicationData> <publicationCode>im</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>fp</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>card</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>chph</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>endo</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>cpn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>skin</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>hemn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>idprac</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>mdsurg</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>oncr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>nr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle>Neurology Reviews</journalTitle> <journalFullTitle>Neurology Reviews</journalFullTitle> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>pn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>ob</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>mdemed</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement/> </publicationData> <publicationData> <publicationCode>rn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> </publications_g> <publications> <term canonical="true">21</term> <term>15</term> <term>5</term> <term>6</term> <term>34</term> <term>9</term> <term>13</term> <term>18</term> <term>20</term> <term>52226</term> <term>31</term> <term>22</term> <term>25</term> <term>23</term> <term>58877</term> <term>26</term> </publications> <sections> <term canonical="true">39313</term> </sections> <topics> <term canonical="true">38029</term> <term>278</term> </topics> <links> <link> <itemClass qcode="ninat:picture"/> <altRep contenttype="image/jpeg">images/24012878.jpg</altRep> <description role="drol:caption"/> <description role="drol:credit">Dr. Wilson</description> </link> <link> <itemClass qcode="ninat:picture"/> <altRep contenttype="image/jpeg">images/24012879.jpg</altRep> <description role="drol:caption"/> <description role="drol:credit">Dr. Wilson</description> </link> </links> </header> <itemSet> <newsItem> <itemMeta> <itemRole>Main</itemRole> <itemClass>text</itemClass> <title>Are Women Better Doctors Than Men?</title> <deck/> </itemMeta> <itemContent> <p><br/><br/><em>This transcript has been edited for clarity</em>.</p> <p>It’s a battle of the sexes today as we dive into a paper that makes you say, “Wow, what an interesting study” and also “Boy, am I glad I didn’t do that study.” That’s because studies like this are always somewhat fraught; they say something about medicine but also something about society — and that makes this a bit precarious. But that’s never stopped us before. So, let’s go ahead and try to answer the question: Do women make better doctors than men?</p> <p>On the surface, this question seems nearly impossible to answer. It’s too broad; what does it mean to be a “better” doctor? At first blush it seems that there are just too many variables to control for here: the type of doctor, the type of patient, the clinical scenario, and so on.<br/><br/>But this <span class="Hyperlink"><a href="https://www.acpjournals.org/doi/10.7326/M23-3163">study</a></span>, “Comparison of hospital mortality and readmission rates by physician and patient sex,” which appears in <em>Annals of Internal Medicine</em>, uses a fairly ingenious method to cut through all the bias by leveraging two simple facts: First, hospital medicine is largely conducted by hospitalists these days; second, due to the shift-based nature of hospitalist work, the hospitalist you get when you are admitted to the hospital is pretty much random.<br/><br/>In other words, if you are admitted to the hospital for an acute illness and get a hospitalist as your attending, you have no control over whether it is a man or a woman. Is this a randomized trial? No, but it’s not bad.<br/><br/>Researchers used Medicare claims data to identify adults over age 65 who had nonelective hospital admissions throughout the United States. The claims revealed the sex of the patient and the name of the attending physician. By linking to a medical provider database, they could determine the sex of the provider.<br/><br/>The goal was to look at outcomes across four dyads:</p> <ul class="body"> <li>Male patient – male doctor</li> <li>Male patient – female doctor</li> <li>Female patient – male doctor</li> <li>Female patient – female doctor</li> </ul> <p>The primary outcome was 30-day mortality.<br/><br/>I told you that focusing on hospitalists produces some pseudorandomization, but let’s look at the data to be sure. Just under a million patients were treated by approximately 50,000 physicians, 30% of whom were female. And, though female patients and male patients differed, they did not differ with respect to the sex of their hospitalist. So, by physician sex, patients were similar in mean age, race, ethnicity, household income, eligibility for Medicaid, and comorbid conditions. The authors even created a “predicted mortality” score which was similar across the groups as well.<br/><br/>[[{"fid":"301165","view_mode":"medstat_image_full_text","fields":{"format":"medstat_image_full_text","field_file_image_alt_text[und][0][value]":"Baseline characteristics","field_file_image_credit[und][0][value]":"Dr. Wilson","field_file_image_caption[und][0][value]":""},"type":"media","attributes":{"class":"media-element file-medstat_image_full_text"}}]]<br/><br/>Now, the female physicians were a bit different from the male physicians. The female hospitalists were slightly more likely to have an osteopathic degree, had slightly fewer admissions per year, and were a bit younger.<br/><br/>So, we have broadly similar patients regardless of who their hospitalist was, but hospitalists differ by factors other than their sex. Fine.<br/><br/>I’ve graphed the results here. <span class="tag metaDescription">Female patients had a significantly lower 30-day mortality rate than male patients, but they fared even better when cared for by female doctors compared with male doctors. There wasn’t a particularly strong influence of physician sex on outcomes for male patients. The secondary outcome, 30-day hospital readmission, showed a similar trend.</span><br/><br/>[[{"fid":"301166","view_mode":"medstat_image_full_text","fields":{"format":"medstat_image_full_text","field_file_image_alt_text[und][0][value]":"Outcomes","field_file_image_credit[und][0][value]":"Dr. Wilson","field_file_image_caption[und][0][value]":""},"type":"media","attributes":{"class":"media-element file-medstat_image_full_text"}}]]<br/><br/>This is a relatively small effect, to be sure, but if you multiply it across the millions of hospitalist admissions per year, you can start to put up some real numbers.<br/><br/>So, what is going on here? I see four broad buckets of possibilities.<br/><br/>Let’s start with the obvious explanation: Women, on average, are better doctors than men. I am married to a woman doctor, and based on my personal experience, this explanation is undoubtedly true. But why would that be?<br/><br/>The authors cite <span class="Hyperlink"><a href="https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3690315/">data that suggest</a></span> that female physicians are less likely than male physicians to dismiss patient concerns — and in particular, the concerns of female patients — perhaps leading to fewer missed diagnoses. But this is impossible to measure with administrative data, so this study can no more tell us whether these female hospitalists are more attentive than their male counterparts than it can suggest that the benefit is mediated by the shorter average height of female physicians. Perhaps the key is being closer to the patient?<br/><br/>The second possibility here is that this has nothing to do with the sex of the physician at all; it has to do with those other things that associate with the sex of the physician. We know, for example, that the female physicians saw fewer patients per year than the male physicians, but the study authors adjusted for this in the statistical models. Still, other unmeasured factors (confounders) could be present. By the way, confounders wouldn’t necessarily change the primary finding — you are better off being cared for by female physicians. It’s just not because they are female; it’s a convenient marker for some other quality, such as age.<br/><br/>The third possibility is that the study represents a phenomenon called collider bias. The idea here is that physicians only get into the study if they are hospitalists, and the quality of physicians who choose to become a hospitalist may differ by sex. When deciding on a specialty, a talented resident considering certain lifestyle issues may find hospital medicine particularly attractive — and that draw toward a more lifestyle-friendly specialty may differ by sex, as <span class="Hyperlink"><a href="https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/647734">some prior studies have shown</a></span>. If true, the pool of women hospitalists may be better than their male counterparts because male physicians of that caliber don’t become hospitalists.<br/><br/>Okay, don’t write in. I’m just trying to cite examples of how to think about collider bias. I can’t prove that this is the case, and in fact the authors do a sensitivity analysis of all physicians, not just hospitalists, and show the same thing. So this is probably not true, but epidemiology is fun, right?<br/><br/>And the fourth possibility: This is nothing but statistical noise. The effect size is incredibly small and just on the border of statistical significance. Especially when you’re working with very large datasets like this, you’ve got to be really careful about overinterpreting statistically significant findings that are nevertheless of small magnitude.<br/><br/>Regardless, it’s an interesting study, one that made me think and, of course, worry a bit about how I would present it. Forgive me if I’ve been indelicate in handling the complex issues of sex, gender, and society here. But I’m not sure what you expect; after all, I’m only a male doctor.<span class="end"/></p> <p> <em>Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.</em> </p> <p> <em>A version of this article appeared on <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/1000715">Medscape.com</a></span>.</em> </p> </itemContent> </newsItem> <newsItem> <itemMeta> <itemRole>teaser</itemRole> <itemClass>text</itemClass> <title/> <deck/> </itemMeta> <itemContent> </itemContent> </newsItem> </itemSet></root>
Tiny Doses of Metabolically Armed CAR T Show Benefits
“Our study showed a manageable safety profile in r/r DLBCL/B-ALL, with promising breakthrough efficacy of a 100% complete remission in all dose groups,” said first author Jingjing Ren, MD, PhD, associate director of research and development with Leman Biotech in Shenzhen, China. Dr. Ren presented these findings at the American Association for Cancer Research annual meeting held in San Diego.
While CD19 CAR T-cell therapy has been transformative in the treatment of relapsed B -cell hematological malignancies in recent years, more than half of patients relapse within a year because of inadequate CAR T persistence.
To address the problem, Dr. Ren and her colleagues developed a metabolically armed, interleukin (IL)-10-expressing CAR T-cell product called Meta10-19 for the treatment patients with r/r DLBCL or r/r B-ALL.
According to the authors, the IL-10-expressing CAR T-cells trigger “stem-like memory responses” in various lymphoid organs, which prompt a “robust tumor eradication and durable protection,” and hence, better persistence.
Preclinical studies in mice showed the Meta10-19 CAR T-cells exhibited substantially higher expansion of approximately 100-fold compared with a control CD19 CAR-T product.
Therefore, “we dramatically reduced the dose to approximately 1% to 5% of commercial products for the IL-10-expressing CD19 CAR-T for patients,” coauthor Yugang Guo, PhD, cofounder and president of Leman Biotech said in an interview.
For the ongoing, open-label clinical trial, 12 adult patients with r/r DLBCL or r/r B-ALL and confirmed CD19 expression at a hospital center in China were enrolled between December 2022 and November 2023 and treated in three cohorts, receiving doses that corresponded to 1%, 2.5%, or 5% of the doses of other commercialized CAR-T infusion products.
All patients also underwent lympho-depleting chemotherapy with cyclophosphamide and fludarabine prior to the CAR T-cell infusion.
Six patients had r/r DLBCL and the other six had r/r B-ALL; their median age was 47 and their median time since diagnosis was 1 year.
In the single-arm, intent-to-treat analysis, the treatment induced a complete remission in all 12 patients, as evaluated by PET-CT scan, nuclear magnetic resonance (NMR) spectroscopy, or minimal residual disease assessment of bone marrow.
The median time to best response was 1 month (range 0.5 to 2.2 months).
There were no cases of severe cytokine storm syndrome or neurotoxicity, which are among key limitations with current commercial CAR-T products.
All of the patients continued to have a complete remission at 3 months. Two of the 12 patients, both with B-ALL, experienced relapses, one after 4.7 months and the other at 8 months.
The authors reported that the first treated patient had maintained continuous remission as of 9 months.
In comparison with the much higher full doses of commercial CD19 CAR-T products, only about 50% of patients with DLBCL and 70% of B-ALL patients have been shown to achieve CR at 3 months, the authors reported.
“Our IL-10 expressing CAR-T sustains CR at 3 months post infusion in the context of not following allogeneic hematopoietic stem cell transplant, which suggests IL-10 expressing CAR-T is more resistant to relapse,” Dr. Guo said.
In terms of safety, six patients with DLBCL and four with B-ALL experienced grade 1 cytokine release syndrome (CRS), and two patients with B-ALL developed grade 2 CRS. There were no grade 3 or 4 CRS cases.
One patient with B-ALL developed grade 3 ICANS.
Grade 3-4 cytopenias occurred in most patients, but all were limited to no later than 90 days.
“We observed reduced CRS, with no level 3 or 4, or ICANS,” Dr. Guo said. “There was increased cytopenia, but still manageable, compared with commercial products.”
Of note, the Meta10-19 cells showed efficacy in the extremely low infusion doses even among patients with bulky mass (≥ 7.5 cm) of DLBCL, which is associated with an increased risk of relapse.
One patient had primary central nervous system lymphoma (PCNSL), a rare form of DLBCL that is known to have the worst prognosis of all non-Hodgkin lymphomas.
Due to the unique nature of CNS primary tumors, the CAR T-cell infusion dose was further reduced to 1% of the standard dose for the patient.
The patient maintained complete remission for more than 8 months before relapsing in periphery blood, but not in the CNS, Dr. Guo noted.
“Luckily, this relapse has been easily controlled by chemotherapy, and the patient is maintaining complete remission again now,” Dr. Guo said.
Mechanisms?
Dr. Guo noted that the mechanism believed to explain the improvements despite such low doses is that “IL-10-expressing CAR-T exhibits enhanced proliferation, cytotoxicity, and stem-like antitumor memory due to enhanced metabolic activities of oxidative phosphorylation.”
The authors noted that a key major factor limiting accessibility to CAR-T therapies is the lengthy production cycle and high costs; however, the “extremely low doses of 1% to 5% can significantly reduce the production cycle and cost of CAR T-cell therapies, increasing accessibility,” they wrote in a press statement.
Currently, more than 20 patients have achieved a CR overall, and studies with a larger cohort and longer follow-up are ongoing, Dr. Guo reported.
The research team plans to launch further clinical investigation this year into patients with solid tumors.
Commenting on the study, Hongbo Chi, PhD, the Robert G. Webster Endowed Chair in Immunology at St. Jude Children’s Research Hospital in Memphis, Tennessee, noted that, based on the abstract, “the effects are quite remarkable, considering the therapeutic efficacy observed even at the low dose.
“Results from more patients are needed to fully validate these findings, but the results to date are very encouraging,” he said.
The study was sponsored by Leman Biotech. Dr. Chi had no disclosures to report.
“Our study showed a manageable safety profile in r/r DLBCL/B-ALL, with promising breakthrough efficacy of a 100% complete remission in all dose groups,” said first author Jingjing Ren, MD, PhD, associate director of research and development with Leman Biotech in Shenzhen, China. Dr. Ren presented these findings at the American Association for Cancer Research annual meeting held in San Diego.
While CD19 CAR T-cell therapy has been transformative in the treatment of relapsed B -cell hematological malignancies in recent years, more than half of patients relapse within a year because of inadequate CAR T persistence.
To address the problem, Dr. Ren and her colleagues developed a metabolically armed, interleukin (IL)-10-expressing CAR T-cell product called Meta10-19 for the treatment patients with r/r DLBCL or r/r B-ALL.
According to the authors, the IL-10-expressing CAR T-cells trigger “stem-like memory responses” in various lymphoid organs, which prompt a “robust tumor eradication and durable protection,” and hence, better persistence.
Preclinical studies in mice showed the Meta10-19 CAR T-cells exhibited substantially higher expansion of approximately 100-fold compared with a control CD19 CAR-T product.
Therefore, “we dramatically reduced the dose to approximately 1% to 5% of commercial products for the IL-10-expressing CD19 CAR-T for patients,” coauthor Yugang Guo, PhD, cofounder and president of Leman Biotech said in an interview.
For the ongoing, open-label clinical trial, 12 adult patients with r/r DLBCL or r/r B-ALL and confirmed CD19 expression at a hospital center in China were enrolled between December 2022 and November 2023 and treated in three cohorts, receiving doses that corresponded to 1%, 2.5%, or 5% of the doses of other commercialized CAR-T infusion products.
All patients also underwent lympho-depleting chemotherapy with cyclophosphamide and fludarabine prior to the CAR T-cell infusion.
Six patients had r/r DLBCL and the other six had r/r B-ALL; their median age was 47 and their median time since diagnosis was 1 year.
In the single-arm, intent-to-treat analysis, the treatment induced a complete remission in all 12 patients, as evaluated by PET-CT scan, nuclear magnetic resonance (NMR) spectroscopy, or minimal residual disease assessment of bone marrow.
The median time to best response was 1 month (range 0.5 to 2.2 months).
There were no cases of severe cytokine storm syndrome or neurotoxicity, which are among key limitations with current commercial CAR-T products.
All of the patients continued to have a complete remission at 3 months. Two of the 12 patients, both with B-ALL, experienced relapses, one after 4.7 months and the other at 8 months.
The authors reported that the first treated patient had maintained continuous remission as of 9 months.
In comparison with the much higher full doses of commercial CD19 CAR-T products, only about 50% of patients with DLBCL and 70% of B-ALL patients have been shown to achieve CR at 3 months, the authors reported.
“Our IL-10 expressing CAR-T sustains CR at 3 months post infusion in the context of not following allogeneic hematopoietic stem cell transplant, which suggests IL-10 expressing CAR-T is more resistant to relapse,” Dr. Guo said.
In terms of safety, six patients with DLBCL and four with B-ALL experienced grade 1 cytokine release syndrome (CRS), and two patients with B-ALL developed grade 2 CRS. There were no grade 3 or 4 CRS cases.
One patient with B-ALL developed grade 3 ICANS.
Grade 3-4 cytopenias occurred in most patients, but all were limited to no later than 90 days.
“We observed reduced CRS, with no level 3 or 4, or ICANS,” Dr. Guo said. “There was increased cytopenia, but still manageable, compared with commercial products.”
Of note, the Meta10-19 cells showed efficacy in the extremely low infusion doses even among patients with bulky mass (≥ 7.5 cm) of DLBCL, which is associated with an increased risk of relapse.
One patient had primary central nervous system lymphoma (PCNSL), a rare form of DLBCL that is known to have the worst prognosis of all non-Hodgkin lymphomas.
Due to the unique nature of CNS primary tumors, the CAR T-cell infusion dose was further reduced to 1% of the standard dose for the patient.
The patient maintained complete remission for more than 8 months before relapsing in periphery blood, but not in the CNS, Dr. Guo noted.
“Luckily, this relapse has been easily controlled by chemotherapy, and the patient is maintaining complete remission again now,” Dr. Guo said.
Mechanisms?
Dr. Guo noted that the mechanism believed to explain the improvements despite such low doses is that “IL-10-expressing CAR-T exhibits enhanced proliferation, cytotoxicity, and stem-like antitumor memory due to enhanced metabolic activities of oxidative phosphorylation.”
The authors noted that a key major factor limiting accessibility to CAR-T therapies is the lengthy production cycle and high costs; however, the “extremely low doses of 1% to 5% can significantly reduce the production cycle and cost of CAR T-cell therapies, increasing accessibility,” they wrote in a press statement.
Currently, more than 20 patients have achieved a CR overall, and studies with a larger cohort and longer follow-up are ongoing, Dr. Guo reported.
The research team plans to launch further clinical investigation this year into patients with solid tumors.
Commenting on the study, Hongbo Chi, PhD, the Robert G. Webster Endowed Chair in Immunology at St. Jude Children’s Research Hospital in Memphis, Tennessee, noted that, based on the abstract, “the effects are quite remarkable, considering the therapeutic efficacy observed even at the low dose.
“Results from more patients are needed to fully validate these findings, but the results to date are very encouraging,” he said.
The study was sponsored by Leman Biotech. Dr. Chi had no disclosures to report.
“Our study showed a manageable safety profile in r/r DLBCL/B-ALL, with promising breakthrough efficacy of a 100% complete remission in all dose groups,” said first author Jingjing Ren, MD, PhD, associate director of research and development with Leman Biotech in Shenzhen, China. Dr. Ren presented these findings at the American Association for Cancer Research annual meeting held in San Diego.
While CD19 CAR T-cell therapy has been transformative in the treatment of relapsed B -cell hematological malignancies in recent years, more than half of patients relapse within a year because of inadequate CAR T persistence.
To address the problem, Dr. Ren and her colleagues developed a metabolically armed, interleukin (IL)-10-expressing CAR T-cell product called Meta10-19 for the treatment patients with r/r DLBCL or r/r B-ALL.
According to the authors, the IL-10-expressing CAR T-cells trigger “stem-like memory responses” in various lymphoid organs, which prompt a “robust tumor eradication and durable protection,” and hence, better persistence.
Preclinical studies in mice showed the Meta10-19 CAR T-cells exhibited substantially higher expansion of approximately 100-fold compared with a control CD19 CAR-T product.
Therefore, “we dramatically reduced the dose to approximately 1% to 5% of commercial products for the IL-10-expressing CD19 CAR-T for patients,” coauthor Yugang Guo, PhD, cofounder and president of Leman Biotech said in an interview.
For the ongoing, open-label clinical trial, 12 adult patients with r/r DLBCL or r/r B-ALL and confirmed CD19 expression at a hospital center in China were enrolled between December 2022 and November 2023 and treated in three cohorts, receiving doses that corresponded to 1%, 2.5%, or 5% of the doses of other commercialized CAR-T infusion products.
All patients also underwent lympho-depleting chemotherapy with cyclophosphamide and fludarabine prior to the CAR T-cell infusion.
Six patients had r/r DLBCL and the other six had r/r B-ALL; their median age was 47 and their median time since diagnosis was 1 year.
In the single-arm, intent-to-treat analysis, the treatment induced a complete remission in all 12 patients, as evaluated by PET-CT scan, nuclear magnetic resonance (NMR) spectroscopy, or minimal residual disease assessment of bone marrow.
The median time to best response was 1 month (range 0.5 to 2.2 months).
There were no cases of severe cytokine storm syndrome or neurotoxicity, which are among key limitations with current commercial CAR-T products.
All of the patients continued to have a complete remission at 3 months. Two of the 12 patients, both with B-ALL, experienced relapses, one after 4.7 months and the other at 8 months.
The authors reported that the first treated patient had maintained continuous remission as of 9 months.
In comparison with the much higher full doses of commercial CD19 CAR-T products, only about 50% of patients with DLBCL and 70% of B-ALL patients have been shown to achieve CR at 3 months, the authors reported.
“Our IL-10 expressing CAR-T sustains CR at 3 months post infusion in the context of not following allogeneic hematopoietic stem cell transplant, which suggests IL-10 expressing CAR-T is more resistant to relapse,” Dr. Guo said.
In terms of safety, six patients with DLBCL and four with B-ALL experienced grade 1 cytokine release syndrome (CRS), and two patients with B-ALL developed grade 2 CRS. There were no grade 3 or 4 CRS cases.
One patient with B-ALL developed grade 3 ICANS.
Grade 3-4 cytopenias occurred in most patients, but all were limited to no later than 90 days.
“We observed reduced CRS, with no level 3 or 4, or ICANS,” Dr. Guo said. “There was increased cytopenia, but still manageable, compared with commercial products.”
Of note, the Meta10-19 cells showed efficacy in the extremely low infusion doses even among patients with bulky mass (≥ 7.5 cm) of DLBCL, which is associated with an increased risk of relapse.
One patient had primary central nervous system lymphoma (PCNSL), a rare form of DLBCL that is known to have the worst prognosis of all non-Hodgkin lymphomas.
Due to the unique nature of CNS primary tumors, the CAR T-cell infusion dose was further reduced to 1% of the standard dose for the patient.
The patient maintained complete remission for more than 8 months before relapsing in periphery blood, but not in the CNS, Dr. Guo noted.
“Luckily, this relapse has been easily controlled by chemotherapy, and the patient is maintaining complete remission again now,” Dr. Guo said.
Mechanisms?
Dr. Guo noted that the mechanism believed to explain the improvements despite such low doses is that “IL-10-expressing CAR-T exhibits enhanced proliferation, cytotoxicity, and stem-like antitumor memory due to enhanced metabolic activities of oxidative phosphorylation.”
The authors noted that a key major factor limiting accessibility to CAR-T therapies is the lengthy production cycle and high costs; however, the “extremely low doses of 1% to 5% can significantly reduce the production cycle and cost of CAR T-cell therapies, increasing accessibility,” they wrote in a press statement.
Currently, more than 20 patients have achieved a CR overall, and studies with a larger cohort and longer follow-up are ongoing, Dr. Guo reported.
The research team plans to launch further clinical investigation this year into patients with solid tumors.
Commenting on the study, Hongbo Chi, PhD, the Robert G. Webster Endowed Chair in Immunology at St. Jude Children’s Research Hospital in Memphis, Tennessee, noted that, based on the abstract, “the effects are quite remarkable, considering the therapeutic efficacy observed even at the low dose.
“Results from more patients are needed to fully validate these findings, but the results to date are very encouraging,” he said.
The study was sponsored by Leman Biotech. Dr. Chi had no disclosures to report.
<!--$RCSfile: InCopy_agile.xsl,v $ $Revision: 1.35 $-->
<!--$RCSfile: drupal.xsl,v $ $Revision: 1.7 $-->
<root generator="drupal.xsl" gversion="1.7"> <header> <fileName>167804</fileName> <TBEID>0C04FB94.SIG</TBEID> <TBUniqueIdentifier>MD_0C04FB94</TBUniqueIdentifier> <newsOrJournal>News</newsOrJournal> <publisherName>Frontline Medical Communications</publisherName> <storyname>AACR_Metabolic CAR-T Therapy</storyname> <articleType>2</articleType> <TBLocation>QC Done-All Pubs</TBLocation> <QCDate>20240423T101429</QCDate> <firstPublished>20240423T101437</firstPublished> <LastPublished>20240423T101437</LastPublished> <pubStatus qcode="stat:"/> <embargoDate/> <killDate/> <CMSDate>20240423T101436</CMSDate> <articleSource>FROM AACR 2024 </articleSource> <facebookInfo/> <meetingNumber>2976-24</meetingNumber> <byline>Nancy A. Melville</byline> <bylineText>NANCY A. MELVILLE</bylineText> <bylineFull>NANCY A. MELVILLE</bylineFull> <bylineTitleText>MDedge News</bylineTitleText> <USOrGlobal/> <wireDocType/> <newsDocType/> <journalDocType/> <linkLabel/> <pageRange/> <citation/> <quizID/> <indexIssueDate/> <itemClass qcode="ninat:text"/> <provider qcode="provider:imng"> <name>IMNG Medical Media</name> <rightsInfo> <copyrightHolder> <name>Frontline Medical News</name> </copyrightHolder> <copyrightNotice>Copyright (c) 2015 Frontline Medical News, a Frontline Medical Communications Inc. company. All rights reserved. This material may not be published, broadcast, copied, or otherwise reproduced or distributed without the prior written permission of Frontline Medical Communications Inc.</copyrightNotice> </rightsInfo> </provider> <abstract/> <metaDescription>A novel CD19 chimeric antigen responder (CAR) T-cell therapy administered in exceptionally low doses and designed to reinvigorate exhausted T-cells shows impres</metaDescription> <articlePDF/> <teaserImage/> <teaser>The IL-10-expressing Meta10-19 CAR T-cell therapy improved outcomes in B-ALL and DLBCL at doses 5% and lower of standard CAR T products.</teaser> <title>Tiny Doses of Metabolically Armed CAR T Show Benefits</title> <deck/> <disclaimer/> <AuthorList/> <articleURL/> <doi/> <pubMedID/> <publishXMLStatus/> <publishXMLVersion>1</publishXMLVersion> <useEISSN>0</useEISSN> <urgency/> <pubPubdateYear/> <pubPubdateMonth/> <pubPubdateDay/> <pubVolume/> <pubNumber/> <wireChannels/> <primaryCMSID/> <CMSIDs/> <keywords/> <seeAlsos/> <publications_g> <publicationData> <publicationCode>hemn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> </publications_g> <publications> <term canonical="true">18</term> </publications> <sections> <term canonical="true">53</term> <term>39313</term> </sections> <topics> <term canonical="true">195</term> <term>179</term> <term>61821</term> <term>49434</term> </topics> <links/> </header> <itemSet> <newsItem> <itemMeta> <itemRole>Main</itemRole> <itemClass>text</itemClass> <title>Tiny Doses of Metabolically Armed CAR T Show Benefits</title> <deck/> </itemMeta> <itemContent> <p> <span class="tag metaDescription">A novel CD19 chimeric antigen responder (CAR) T-cell therapy administered in exceptionally low doses and designed to reinvigorate exhausted T-cells shows impressive early results in the treatment of patients with relapsed or refractory (r/r) diffuse large B-cell lymphoma (DLBCL) and B-cell acute lymphoblastic leukemia (B-ALL).</span> </p> <p>“Our study showed a manageable safety profile in r/r DLBCL/B-ALL, with promising breakthrough efficacy of a 100% complete remission in all dose groups,” said first author Jingjing Ren, MD, PhD, associate director of research and development with Leman Biotech in Shenzhen, China. Dr. Ren <span class="Hyperlink"><a href="https://www.abstractsonline.com/pp8/#!/20272/presentation/11336">presented these findings</a></span> at the American Association for Cancer Research annual meeting held in San Diego.<br/><br/>While CD19 CAR T-cell therapy has been transformative in the treatment of relapsed B -cell hematological malignancies in recent years, more than half of patients relapse within a year because of inadequate CAR T persistence.<br/><br/>To address the problem, Dr. Ren and her colleagues developed a metabolically armed, interleukin (IL)-10-expressing CAR T-cell product called Meta10-19 for the treatment patients with r/r DLBCL or r/r B-ALL.<br/><br/>According to the authors, the IL-10-expressing CAR T-cells trigger “stem-like memory responses” in various lymphoid organs, which prompt a “robust tumor eradication and durable protection,” and hence, better persistence. <br/><br/>Preclinical studies in mice showed the Meta10-19 CAR T-cells exhibited substantially higher expansion of approximately 100-fold compared with a control CD19 CAR-T product.<br/><br/>Therefore, “we dramatically reduced the dose to approximately 1% to 5% of commercial products for the IL-10-expressing CD19 CAR-T for patients,” coauthor Yugang Guo, PhD, cofounder and president of Leman Biotech said in an interview.<br/><br/>For the ongoing, open-label clinical trial, 12 adult patients with r/r DLBCL or r/r B-ALL and confirmed CD19 expression at a hospital center in China were enrolled between December 2022 and November 2023 and treated in three cohorts, receiving doses that corresponded to 1%, 2.5%, or 5% of the doses of other commercialized CAR-T infusion products.<br/><br/>All patients also underwent lympho-depleting chemotherapy with cyclophosphamide and fludarabine prior to the CAR T-cell infusion. <br/><br/>Six patients had r/r DLBCL and the other six had r/r B-ALL; their median age was 47 and their median time since diagnosis was 1 year. <br/><br/>In the single-arm, intent-to-treat analysis, the treatment induced a complete remission in all 12 patients, as evaluated by PET-CT scan, nuclear magnetic resonance (NMR) spectroscopy, or minimal residual disease assessment of bone marrow. <br/><br/>The median time to best response was 1 month (range 0.5 to 2.2 months).<br/><br/>There were no cases of severe cytokine storm syndrome or neurotoxicity, which are among key limitations with current commercial CAR-T products.<br/><br/>All of the patients continued to have a complete remission at 3 months. Two of the 12 patients, both with B-ALL, experienced relapses, one after 4.7 months and the other at 8 months.<br/><br/>The authors reported that the first treated patient had maintained continuous remission as of 9 months.<br/><br/>In comparison with the much higher full doses of commercial CD19 CAR-T products, only about 50% of patients with DLBCL and 70% of B-ALL patients have been shown to achieve CR at 3 months, the authors reported.<br/><br/>“Our IL-10 expressing CAR-T sustains CR at 3 months post infusion in the context of not following allogeneic hematopoietic stem cell transplant, which suggests IL-10 expressing CAR-T is more resistant to relapse,” Dr. Guo said.<br/><br/>In terms of safety, six patients with DLBCL and four with B-ALL experienced grade 1 cytokine release syndrome (CRS), and two patients with B-ALL developed grade 2 CRS. There were no grade 3 or 4 CRS cases.<br/><br/>One patient with B-ALL developed grade 3 ICANS.<br/><br/>Grade 3-4 cytopenias occurred in most patients, but all were limited to no later than 90 days.<br/><br/>“We observed reduced CRS, with no level 3 or 4, or ICANS,” Dr. Guo said. “There was increased cytopenia, but still manageable, compared with commercial products.”<br/><br/>Of note, the Meta10-19 cells showed efficacy in the extremely low infusion doses even among patients with bulky mass (≥ 7.5 cm) of DLBCL, which is associated with an increased risk of relapse.<br/><br/>One patient had primary central nervous system lymphoma (PCNSL), a rare form of DLBCL that is known to have the worst prognosis of all non-Hodgkin lymphomas. <br/><br/>Due to the unique nature of CNS primary tumors, the CAR T-cell infusion dose was further reduced to 1% of the standard dose for the patient. <br/><br/>The patient maintained complete remission for more than 8 months before relapsing in periphery blood, but not in the CNS, Dr. Guo noted. <br/><br/>“Luckily, this relapse has been easily controlled by chemotherapy, and the patient is maintaining complete remission again now,” Dr. Guo said.<br/><br/></p> <h2>Mechanisms?</h2> <p>Dr. Guo noted that the mechanism believed to explain the improvements despite such low doses is that “IL-10-expressing CAR-T exhibits enhanced proliferation, cytotoxicity, and stem-like antitumor memory due to enhanced metabolic activities of oxidative phosphorylation.” <br/><br/>The authors noted that a key major factor limiting accessibility to CAR-T therapies is the lengthy production cycle and high costs; however, the “extremely low doses of 1% to 5% can significantly reduce the production cycle and cost of CAR T-cell therapies, increasing accessibility,” they wrote in a press statement.<br/><br/>Currently, more than 20 patients have achieved a CR overall, and studies with a larger cohort and longer follow-up are ongoing, Dr. Guo reported. <br/><br/>The research team plans to launch further clinical investigation this year into patients with solid tumors.<br/><br/>Commenting on the study, Hongbo Chi, PhD, the Robert G. Webster Endowed Chair in Immunology at St. Jude Children’s Research Hospital in Memphis, Tennessee, noted that, based on the abstract, “the effects are quite remarkable, considering the therapeutic efficacy observed even at the low dose.<br/><br/>“Results from more patients are needed to fully validate these findings, but the results to date are very encouraging,” he said. <br/><br/>The study was sponsored by Leman Biotech. Dr. Chi had no disclosures to report.</p> </itemContent> </newsItem> <newsItem> <itemMeta> <itemRole>teaser</itemRole> <itemClass>text</itemClass> <title/> <deck/> </itemMeta> <itemContent> </itemContent> </newsItem> </itemSet></root>
FROM AACR 2024
Weighing the Benefits of Integrating AI-based Clinical Notes Into Your Practice
Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided attention and personalized care. In a recent X post, Stuart Blitz, COO and co-founder of Hone Health, sparked a thought-provoking conversation. “The problem with US healthcare is physicians are burned out since they spend way too much time charting, not enough with patients,” he wrote. “If you created a health system that did zero charting, you’d attract the best physicians and all patients would go there. Who is working on this?”
This resonates with many in the medical community, myself included, because the strain of extensive documentation detracts from patient care. Having worked in both large and small healthcare systems, I know the burden of extensive charting is a palpable challenge, often detracting from the time we can devote to our patients.
The first part of this two-part series examines the overarching benefits of artificial intelligence (AI)–based clinical documentation in modern healthcare, a field witnessing a paradigm shift thanks to advancements in AI.
Transformative Evolution of Clinical Documentation
The transition from manual documentation to AI-driven solutions marks a significant shift in the field, with a number of products in development including Nuance, Abridge, Ambience, ScribeAmerica, 3M, and DeepScribe. These tools use ambient clinical intelligence (ACI) to automate documentation, capturing patient conversations and translating them into structured clinical summaries. This innovation aligns with the vision of reducing charting burdens and enhancing patient-physician interactions.
How does it work? ACI refers to a sophisticated form of AI applied in healthcare settings, particularly focusing on enhancing the clinical documentation process without disrupting the natural flow of the consultation. Here’s a technical yet practical breakdown of ACI and the algorithms it typically employs:
Data capture and processing: ACI systems employ various sensors and processing units, typically integrated into clinical settings. These sensors, like microphones and cameras, gather diverse data such as audio from patient-doctor dialogues and visual cues. This information is then processed in real-time or near–real-time.
Natural language processing (NLP): A core component of ACI is advanced NLP algorithms. These algorithms analyze the captured audio data, transcribing spoken words into text. NLP goes beyond mere transcription; it involves understanding context, extracting relevant medical information (like symptoms, diagnoses, and treatment plans), and interpreting the nuances of human language.
Deep learning: Machine learning, particularly deep-learning techniques, are employed to improve the accuracy of ACI systems continually. These algorithms can learn from vast datasets of clinical interactions, enhancing their ability to transcribe and interpret future conversations accurately. As they learn, they become better at understanding different accents, complex medical terms, and variations in speech patterns.
Integration with electronic health records (EHRs): ACI systems are often designed to integrate seamlessly with existing EHR systems. They can automatically populate patient records with information from patient-clinician interactions, reducing manual entry and potential errors.
Customization and personalization: Many ACI systems offer customizable templates or allow clinicians to tailor documentation workflows. This flexibility ensures that the output aligns with the specific needs and preferences of healthcare providers.
Ethical and privacy considerations: ACI systems must navigate significant ethical and privacy concerns, especially related to patient consent and data security. These systems need to comply with healthcare privacy regulations such as HIPAA. They need to securely manage sensitive patient data and restrict access to authorized personnel only.
Broad-Spectrum Benefits of AI in Documentation
- Reducing clinician burnout: By automating the documentation process, AI tools like DAX Copilot alleviate a significant contributor to physician burnout, enabling clinicians to focus more on patient care.
- Enhanced patient care: With AI handling documentation, clinicians can engage more with their patients, leading to improved care quality and patient satisfaction.
- Data accuracy and quality: AI-driven documentation captures detailed patient encounters accurately, ensuring high-quality and comprehensive medical records.
- Response to the growing need for efficient healthcare: AI-based documentation is a direct response to the growing call for more efficient healthcare practices, where clinicians spend less time on paperwork and more with patients.
The shift toward AI-based clinical documentation represents a critical step in addressing the inefficiencies in healthcare systems. It’s a move towards a more patient-centered approach, where clinicians can focus more on patient care by reducing the time spent on excessive charting. Hopefully, we can integrate these solutions into our clinics at a large enough scale to make such an impact.
In the next column, we will explore in-depth insights from Kenneth Harper at Nuance on the technical implementation of these tools, with DAX as an example.
I would love to read your comments on AI in clinical trials as well as other AI-related topics. Write me at Arturo.ai.medtech@gmail.com or find me on X @DrBonillaOnc.
Dr. Loaiza-Bonilla is the co-founder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr Loaiza-Bonilla serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has served as a consultant for Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, and Guardant; served as a speaker or a member of a speakers bureau for Amgen, Guardant, Eisai, Ipsen, Natera, Merck, Bristol-Myers Squibb, and AstraZeneca. He holds a 5% or greater equity interest in Massive Bio.
A version of this article appeared on Medscape.com.
Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided attention and personalized care. In a recent X post, Stuart Blitz, COO and co-founder of Hone Health, sparked a thought-provoking conversation. “The problem with US healthcare is physicians are burned out since they spend way too much time charting, not enough with patients,” he wrote. “If you created a health system that did zero charting, you’d attract the best physicians and all patients would go there. Who is working on this?”
This resonates with many in the medical community, myself included, because the strain of extensive documentation detracts from patient care. Having worked in both large and small healthcare systems, I know the burden of extensive charting is a palpable challenge, often detracting from the time we can devote to our patients.
The first part of this two-part series examines the overarching benefits of artificial intelligence (AI)–based clinical documentation in modern healthcare, a field witnessing a paradigm shift thanks to advancements in AI.
Transformative Evolution of Clinical Documentation
The transition from manual documentation to AI-driven solutions marks a significant shift in the field, with a number of products in development including Nuance, Abridge, Ambience, ScribeAmerica, 3M, and DeepScribe. These tools use ambient clinical intelligence (ACI) to automate documentation, capturing patient conversations and translating them into structured clinical summaries. This innovation aligns with the vision of reducing charting burdens and enhancing patient-physician interactions.
How does it work? ACI refers to a sophisticated form of AI applied in healthcare settings, particularly focusing on enhancing the clinical documentation process without disrupting the natural flow of the consultation. Here’s a technical yet practical breakdown of ACI and the algorithms it typically employs:
Data capture and processing: ACI systems employ various sensors and processing units, typically integrated into clinical settings. These sensors, like microphones and cameras, gather diverse data such as audio from patient-doctor dialogues and visual cues. This information is then processed in real-time or near–real-time.
Natural language processing (NLP): A core component of ACI is advanced NLP algorithms. These algorithms analyze the captured audio data, transcribing spoken words into text. NLP goes beyond mere transcription; it involves understanding context, extracting relevant medical information (like symptoms, diagnoses, and treatment plans), and interpreting the nuances of human language.
Deep learning: Machine learning, particularly deep-learning techniques, are employed to improve the accuracy of ACI systems continually. These algorithms can learn from vast datasets of clinical interactions, enhancing their ability to transcribe and interpret future conversations accurately. As they learn, they become better at understanding different accents, complex medical terms, and variations in speech patterns.
Integration with electronic health records (EHRs): ACI systems are often designed to integrate seamlessly with existing EHR systems. They can automatically populate patient records with information from patient-clinician interactions, reducing manual entry and potential errors.
Customization and personalization: Many ACI systems offer customizable templates or allow clinicians to tailor documentation workflows. This flexibility ensures that the output aligns with the specific needs and preferences of healthcare providers.
Ethical and privacy considerations: ACI systems must navigate significant ethical and privacy concerns, especially related to patient consent and data security. These systems need to comply with healthcare privacy regulations such as HIPAA. They need to securely manage sensitive patient data and restrict access to authorized personnel only.
Broad-Spectrum Benefits of AI in Documentation
- Reducing clinician burnout: By automating the documentation process, AI tools like DAX Copilot alleviate a significant contributor to physician burnout, enabling clinicians to focus more on patient care.
- Enhanced patient care: With AI handling documentation, clinicians can engage more with their patients, leading to improved care quality and patient satisfaction.
- Data accuracy and quality: AI-driven documentation captures detailed patient encounters accurately, ensuring high-quality and comprehensive medical records.
- Response to the growing need for efficient healthcare: AI-based documentation is a direct response to the growing call for more efficient healthcare practices, where clinicians spend less time on paperwork and more with patients.
The shift toward AI-based clinical documentation represents a critical step in addressing the inefficiencies in healthcare systems. It’s a move towards a more patient-centered approach, where clinicians can focus more on patient care by reducing the time spent on excessive charting. Hopefully, we can integrate these solutions into our clinics at a large enough scale to make such an impact.
In the next column, we will explore in-depth insights from Kenneth Harper at Nuance on the technical implementation of these tools, with DAX as an example.
I would love to read your comments on AI in clinical trials as well as other AI-related topics. Write me at Arturo.ai.medtech@gmail.com or find me on X @DrBonillaOnc.
Dr. Loaiza-Bonilla is the co-founder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr Loaiza-Bonilla serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has served as a consultant for Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, and Guardant; served as a speaker or a member of a speakers bureau for Amgen, Guardant, Eisai, Ipsen, Natera, Merck, Bristol-Myers Squibb, and AstraZeneca. He holds a 5% or greater equity interest in Massive Bio.
A version of this article appeared on Medscape.com.
Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided attention and personalized care. In a recent X post, Stuart Blitz, COO and co-founder of Hone Health, sparked a thought-provoking conversation. “The problem with US healthcare is physicians are burned out since they spend way too much time charting, not enough with patients,” he wrote. “If you created a health system that did zero charting, you’d attract the best physicians and all patients would go there. Who is working on this?”
This resonates with many in the medical community, myself included, because the strain of extensive documentation detracts from patient care. Having worked in both large and small healthcare systems, I know the burden of extensive charting is a palpable challenge, often detracting from the time we can devote to our patients.
The first part of this two-part series examines the overarching benefits of artificial intelligence (AI)–based clinical documentation in modern healthcare, a field witnessing a paradigm shift thanks to advancements in AI.
Transformative Evolution of Clinical Documentation
The transition from manual documentation to AI-driven solutions marks a significant shift in the field, with a number of products in development including Nuance, Abridge, Ambience, ScribeAmerica, 3M, and DeepScribe. These tools use ambient clinical intelligence (ACI) to automate documentation, capturing patient conversations and translating them into structured clinical summaries. This innovation aligns with the vision of reducing charting burdens and enhancing patient-physician interactions.
How does it work? ACI refers to a sophisticated form of AI applied in healthcare settings, particularly focusing on enhancing the clinical documentation process without disrupting the natural flow of the consultation. Here’s a technical yet practical breakdown of ACI and the algorithms it typically employs:
Data capture and processing: ACI systems employ various sensors and processing units, typically integrated into clinical settings. These sensors, like microphones and cameras, gather diverse data such as audio from patient-doctor dialogues and visual cues. This information is then processed in real-time or near–real-time.
Natural language processing (NLP): A core component of ACI is advanced NLP algorithms. These algorithms analyze the captured audio data, transcribing spoken words into text. NLP goes beyond mere transcription; it involves understanding context, extracting relevant medical information (like symptoms, diagnoses, and treatment plans), and interpreting the nuances of human language.
Deep learning: Machine learning, particularly deep-learning techniques, are employed to improve the accuracy of ACI systems continually. These algorithms can learn from vast datasets of clinical interactions, enhancing their ability to transcribe and interpret future conversations accurately. As they learn, they become better at understanding different accents, complex medical terms, and variations in speech patterns.
Integration with electronic health records (EHRs): ACI systems are often designed to integrate seamlessly with existing EHR systems. They can automatically populate patient records with information from patient-clinician interactions, reducing manual entry and potential errors.
Customization and personalization: Many ACI systems offer customizable templates or allow clinicians to tailor documentation workflows. This flexibility ensures that the output aligns with the specific needs and preferences of healthcare providers.
Ethical and privacy considerations: ACI systems must navigate significant ethical and privacy concerns, especially related to patient consent and data security. These systems need to comply with healthcare privacy regulations such as HIPAA. They need to securely manage sensitive patient data and restrict access to authorized personnel only.
Broad-Spectrum Benefits of AI in Documentation
- Reducing clinician burnout: By automating the documentation process, AI tools like DAX Copilot alleviate a significant contributor to physician burnout, enabling clinicians to focus more on patient care.
- Enhanced patient care: With AI handling documentation, clinicians can engage more with their patients, leading to improved care quality and patient satisfaction.
- Data accuracy and quality: AI-driven documentation captures detailed patient encounters accurately, ensuring high-quality and comprehensive medical records.
- Response to the growing need for efficient healthcare: AI-based documentation is a direct response to the growing call for more efficient healthcare practices, where clinicians spend less time on paperwork and more with patients.
The shift toward AI-based clinical documentation represents a critical step in addressing the inefficiencies in healthcare systems. It’s a move towards a more patient-centered approach, where clinicians can focus more on patient care by reducing the time spent on excessive charting. Hopefully, we can integrate these solutions into our clinics at a large enough scale to make such an impact.
In the next column, we will explore in-depth insights from Kenneth Harper at Nuance on the technical implementation of these tools, with DAX as an example.
I would love to read your comments on AI in clinical trials as well as other AI-related topics. Write me at Arturo.ai.medtech@gmail.com or find me on X @DrBonillaOnc.
Dr. Loaiza-Bonilla is the co-founder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr Loaiza-Bonilla serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has served as a consultant for Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, and Guardant; served as a speaker or a member of a speakers bureau for Amgen, Guardant, Eisai, Ipsen, Natera, Merck, Bristol-Myers Squibb, and AstraZeneca. He holds a 5% or greater equity interest in Massive Bio.
A version of this article appeared on Medscape.com.
<!--$RCSfile: InCopy_agile.xsl,v $ $Revision: 1.35 $-->
<!--$RCSfile: drupal.xsl,v $ $Revision: 1.7 $-->
<root generator="drupal.xsl" gversion="1.7"> <header> <fileName>167723</fileName> <TBEID>0C04F96F.SIG</TBEID> <TBUniqueIdentifier>MD_0C04F96F</TBUniqueIdentifier> <newsOrJournal>News</newsOrJournal> <publisherName>Frontline Medical Communications</publisherName> <storyname/> <articleType>353</articleType> <TBLocation>QC Done-All Pubs</TBLocation> <QCDate>20240422T171622</QCDate> <firstPublished>20240422T173902</firstPublished> <LastPublished>20240422T173902</LastPublished> <pubStatus qcode="stat:"/> <embargoDate/> <killDate/> <CMSDate>20240422T173902</CMSDate> <articleSource/> <facebookInfo/> <meetingNumber/> <byline>Arturo Loaiza-Bonilla, MD</byline> <bylineText>ARTURO LOAIZA-BONILLA, MD</bylineText> <bylineFull>ARTURO LOAIZA-BONILLA, MD</bylineFull> <bylineTitleText/> <USOrGlobal/> <wireDocType/> <newsDocType>Opinion</newsDocType> <journalDocType/> <linkLabel/> <pageRange/> <citation/> <quizID/> <indexIssueDate/> <itemClass qcode="ninat:text"/> <provider qcode="provider:imng"> <name>IMNG Medical Media</name> <rightsInfo> <copyrightHolder> <name>Frontline Medical News</name> </copyrightHolder> <copyrightNotice>Copyright (c) 2015 Frontline Medical News, a Frontline Medical Communications Inc. company. All rights reserved. This material may not be published, broadcast, copied, or otherwise reproduced or distributed without the prior written permission of Frontline Medical Communications Inc.</copyrightNotice> </rightsInfo> </provider> <abstract/> <metaDescription>Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided atte</metaDescription> <articlePDF/> <teaserImage/> <teaser>Artificial intelligence expert Arturo Loaiza-Bonilla, MD, discusses the benefits of AI-based clinical notes.</teaser> <title>Weighing the Benefits of Integrating AI-based Clinical Notes Into Your Practice</title> <deck/> <disclaimer/> <AuthorList/> <articleURL/> <doi/> <pubMedID/> <publishXMLStatus/> <publishXMLVersion>1</publishXMLVersion> <useEISSN>0</useEISSN> <urgency/> <pubPubdateYear/> <pubPubdateMonth/> <pubPubdateDay/> <pubVolume/> <pubNumber/> <wireChannels/> <primaryCMSID/> <CMSIDs/> <keywords/> <seeAlsos/> <publications_g> <publicationData> <publicationCode>oncr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>rn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>pn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>ob</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>nr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle>Neurology Reviews</journalTitle> <journalFullTitle>Neurology Reviews</journalFullTitle> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>mdsurg</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>mdemed</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement/> </publicationData> <publicationData> <publicationCode>mdid</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>im</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>hemn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>fp</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>skin</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>cpn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>endo</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>chph</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>card</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> </publications_g> <publications> <term canonical="true">31</term> <term>26</term> <term>25</term> <term>23</term> <term>22</term> <term>52226</term> <term>58877</term> <term>51892</term> <term>21</term> <term>18</term> <term>15</term> <term>13</term> <term>9</term> <term>34</term> <term>6</term> <term>5</term> </publications> <sections> <term>41022</term> <term canonical="true">52</term> </sections> <topics> <term>278</term> <term canonical="true">38029</term> </topics> <links/> </header> <itemSet> <newsItem> <itemMeta> <itemRole>Main</itemRole> <itemClass>text</itemClass> <title>Weighing the Benefits of Integrating AI-based Clinical Notes Into Your Practice</title> <deck/> </itemMeta> <itemContent> <p>Picture a healthcare system where physicians aren’t bogged down by excessive charting but are instead fully present with their patients, offering undivided attention and personalized care. <a href="https://twitter.com/StuartBlitz/status/1754302729109795224?s=20">In a recent X post</a>, Stuart Blitz, COO and co-founder of Hone Health, sparked a thought-provoking conversation. “The problem with US healthcare is physicians are burned out since they spend way too much time charting, not enough with patients,” he wrote. “If you created a health system that did zero charting, you’d attract the best physicians and all patients would go there. Who is working on this?” </p> <p>This resonates with many in the medical community, myself included, because the strain of extensive documentation detracts from patient care. Having worked in both large and small healthcare systems, I know the burden of extensive charting is a palpable challenge, often detracting from the time we can devote to our patients.<br/><br/>The first part of this two-part series examines the overarching benefits of artificial intelligence (AI)–based clinical documentation in modern healthcare, a field witnessing a paradigm shift thanks to advancements in AI.<br/><br/></p> <h2>Transformative Evolution of Clinical Documentation</h2> <p>The transition from manual documentation to AI-driven solutions marks a significant shift in the field, with a number of products in development including Nuance, Abridge, Ambience, ScribeAmerica, 3M, and DeepScribe. These tools use ambient clinical intelligence (ACI) to automate documentation, capturing patient conversations and translating them into structured clinical summaries. This innovation aligns with the vision of reducing charting burdens and enhancing patient-physician interactions.</p> <p>How does it work? ACI refers to a sophisticated form of AI applied in healthcare settings, particularly focusing on enhancing the clinical documentation process without disrupting the natural flow of the consultation. Here’s a technical yet practical breakdown of ACI and the algorithms it typically employs:<br/><br/><b>Data capture and processing:</b> ACI systems employ various sensors and processing units, typically integrated into clinical settings. These sensors, like microphones and cameras, gather diverse data such as audio from patient-doctor dialogues and visual cues. This information is then processed in real-time or near–real-time.<br/><br/><span class="Strong">Natural language processing (NLP):</span> A core component of ACI is advanced NLP algorithms. These algorithms analyze the captured audio data, transcribing spoken words into text. NLP goes beyond mere transcription; it involves understanding context, extracting relevant medical information (like symptoms, diagnoses, and treatment plans), and interpreting the nuances of human language.<br/><br/><span class="Strong">Deep learning:</span> Machine learning, particularly deep-learning techniques, are employed to improve the accuracy of ACI systems continually. These algorithms can learn from vast datasets of clinical interactions, enhancing their ability to transcribe and interpret future conversations accurately. As they learn, they become better at understanding different accents, complex medical terms, and variations in speech patterns.<br/><br/><span class="Strong">Integration with electronic health records (EHRs):</span> ACI systems are often designed to integrate seamlessly with existing EHR systems. They can automatically populate patient records with information from patient-clinician interactions, reducing manual entry and potential errors.<br/><br/><span class="Strong">Customization and personalization:</span> Many ACI systems offer customizable templates or allow clinicians to tailor documentation workflows. This flexibility ensures that the output aligns with the specific needs and preferences of healthcare providers.<br/><br/><span class="Strong">Ethical and privacy considerations:</span> ACI systems must navigate significant ethical and privacy concerns, especially related to patient consent and data security. These systems need to comply with healthcare privacy regulations such as HIPAA. They need to securely manage sensitive patient data and restrict access to authorized personnel only.<br/><br/></p> <h2>Broad-Spectrum Benefits of AI in Documentation</h2> <ul class="body"> <li><b>Reducing clinician burnout:</b> By automating the documentation process, AI tools like DAX Copilot alleviate a significant contributor to physician burnout, enabling clinicians to focus more on patient care.</li> <li><b>Enhanced patient care:</b> With AI handling documentation, clinicians can engage more with their patients, leading to improved care quality and patient satisfaction.</li> <li><b>Data accuracy and quality:</b> AI-driven documentation captures detailed patient encounters accurately, ensuring high-quality and comprehensive medical records.</li> <li><b>Response to the growing need for efficient healthcare:</b> AI-based documentation is a direct response to the growing call for more efficient healthcare practices, where clinicians spend less time on paperwork and more with patients.</li> </ul> <p>The shift toward AI-based clinical documentation represents a critical step in addressing the inefficiencies in healthcare systems. It’s a move towards a more patient-centered approach, where clinicians can focus more on patient care by reducing the time spent on excessive charting. Hopefully, we can integrate these solutions into our clinics at a large enough scale to make such an impact.<br/><br/>In the next column, we will explore in-depth insights from Kenneth Harper at Nuance on the technical implementation of these tools, with <a href="https://www.nuance.com/healthcare/dragon-ai-clinical-solutions/dax-copilot.html">DAX</a> as an example.<br/><br/>I would love to read your comments on AI in clinical trials as well as other AI-related topics. Write me at <a href="mailto:Arturo.ai.medtech@gmail.com">Arturo.ai.medtech@gmail.com</a> or find me on X <span class="Hyperlink"><a href="https://twitter.com/@DrBonillaOnc">@DrBonillaOnc</a></span>.<span class="end"/></p> <p> <em>Dr. Loaiza-Bonilla is the co-founder and chief medical officer at Massive Bio, a company connecting patients to clinical trials using artificial intelligence. His research and professional interests focus on precision medicine, clinical trial design, digital health, entrepreneurship, and patient advocacy. Dr Loaiza-Bonilla serves as medical director of oncology research at Capital Health in New Jersey, where he maintains a connection to patient care by attending to patients 2 days a week. He has served as a consultant for Verify, PSI CRO, Bayer, AstraZeneca, Cardinal Health, BrightInsight, The Lynx Group, Fresenius, Pfizer, Ipsen, and Guardant; served as a speaker or a member of a speakers bureau for Amgen, Guardant, Eisai, Ipsen, Natera, Merck, Bristol-Myers Squibb, and AstraZeneca. He holds a 5% or greater equity interest in Massive Bio.</em> </p> <p> <em>A version of this article appeared on <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/weighing-benefits-integrating-ai-based-clinical-notes-your-2024a10006r5">Medscape.com</a></span>.</em> </p> </itemContent> </newsItem> <newsItem> <itemMeta> <itemRole>teaser</itemRole> <itemClass>text</itemClass> <title/> <deck/> </itemMeta> <itemContent> </itemContent> </newsItem> </itemSet></root>
New Federal Rule Delivers Workplace Support, Time Off for Pregnant Docs
Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Opportunity Commission (EEOC). The guidelines could prevent women from losing critical career momentum.
The Pregnant Workers Fairness Act (PWFA) aims to help workers balance professional demands with healthy pregnancies. It requires employers to provide reasonable accommodations for a “worker’s known limitations,” including physical or mental conditions associated with “pregnancy, childbirth, or related medical conditions.”
Reasonable accommodations vary but may involve time off to attend healthcare appointments or recover from childbirth, extra breaks during a shift, shorter work hours, or the ability to sit instead of stand. Private and public sector employers, including state and local governments, federal agencies, and employment agencies, must abide by the new guidelines unless they can provide evidence that doing so will cause undue hardship.
Female doctors have historically encountered significant barriers to family planning. Years of training cause them to delay having children, often leading to higher rates of infertility, miscarriage, and pregnancy complications than in the general population.
Some specialties, like surgeons, are particularly at risk, with 42% reporting at least one pregnancy loss. Most surgeons work their regular schedules until delivery despite desiring workload reductions, commonly citing unsupportive workplaces as a reason for not seeking accommodations.
Trauma surgeon Qaali Hussein, MD, became pregnant with her first child during her intern year in 2008. She told this news organization that her residency program didn’t even have a maternity policy at the time, and her male supervisor was certain that motherhood would end her surgical career.
She shared how “women usually waited until the end of their training to get pregnant. No one had ever gotten pregnant during the program and returned from maternity leave. I was the first to do so, so there wasn’t a policy or any program support to say, ‘What can we do to help?’ ”
Dr. Hussein used her vacation and sick time, returning to work 4 weeks after delivery. She had five more children, including twins her chief year and another baby during fellowship training in 2014.
Each subsequent pregnancy was met with the same response from program leadership, she recalled. “They’d say, ‘This is it. You may have been able to do the first and second child, but this one will be impossible.’ ”
After the PWFA regulations first became enforceable in June, the EEOC accepted public feedback. The guidelines received nearly 100,000 comments, spurred mainly by the inclusion of abortion care as a qualifying condition for which an employee could receive accommodations. About 54,000 comments called for abortion to be excluded from the final rule, and 40,000 supported keeping the clause.
The EEOC issued the final rule on April 15. It includes abortion care. However, the updated rule “does not require any employee to have — or not to have — an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions,” the unpublished version of the final rule said. It is scheduled to take effect 60 days after its publication in the Federal Register on April 19.
Increasing Support for Doctor-Moms
The PWFA supplements other EEOC protections, such as pregnancy discrimination under Title VII of the Civil Rights Act of 1964 and access to reasonable accommodations under the Americans with Disabilities Act. In addition, it builds upon Department of Labor regulations, like the PUMP Act for breastfeeding employees and the Family and Medical Leave Act, which provides 12 weeks of unpaid, job-protected leave for the arrival of a child or certain medical conditions.
FMLA applies only to employees who have worked full-time for at least 12 months for an employer with 50 or more employees. Meanwhile, the unpaid, job-protected leave under the PWFA has no waiting period, lowers the required number of employees to 15, and permits accommodations for up to 40 weeks.
Employers are encouraged to honor “common and simple” requests, like using a closer parking space or pumping or nursing at work, without requiring a doctor’s note, the rule said.
Efforts to improve family leave policies for physicians and residents have been gaining traction. In 2021, the American Board of Medical Specialties began requiring its member boards with training programs lasting 2 or more years to allow at least 6 weeks off for parental, caregiver, and medical leave. This time can be taken without exhausting vacation or sick leave or requiring an extension in training. Over half of the 24 member boards permit leave beyond 6 weeks, including the American Boards of Allergy and Immunology, Emergency Medicine, Family Medicine, Radiology, and Surgery.
Estefania Oliveros, MD, MSc, cardiologist and assistant professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, told this news organization that the Accreditation Council for Graduate Medical Education also requires that residents and fellows receive 6 weeks of paid leave.
“We add to that vacation time, so it gives them at least 8 weeks,” she said. The school has created spaces for nursing mothers — something neither she nor Dr. Hussein had access to when breastfeeding — and encourages the attendings to be proactive in excusing pregnant fellows for appointments.
This differs significantly from her fellowship training experience 6 years ago at another institution, where she worked without accommodations until the day before her cesarean delivery. Dr. Oliveros had to use all her vacation time for recovery, returning to the program after 4 weeks instead of the recommended 6.
“And that’s the story you hear all the time. Not because people are ill-intended; I just don’t think the system is designed to accommodate women, so we lose a lot of talent that way,” said Dr. Oliveros, whose 2019 survey in the Journal of the American College of Cardiology called for more support and protections for pregnant doctors.
Both doctors believe the PWFA will be beneficial but only if leadership in the field takes up the cause.
“The cultures of these institutions determine whether women feel safe or even confident enough to have children in medical school or residency,” said Dr. Hussein.
A version of this article appeared on Medscape.com.
Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Opportunity Commission (EEOC). The guidelines could prevent women from losing critical career momentum.
The Pregnant Workers Fairness Act (PWFA) aims to help workers balance professional demands with healthy pregnancies. It requires employers to provide reasonable accommodations for a “worker’s known limitations,” including physical or mental conditions associated with “pregnancy, childbirth, or related medical conditions.”
Reasonable accommodations vary but may involve time off to attend healthcare appointments or recover from childbirth, extra breaks during a shift, shorter work hours, or the ability to sit instead of stand. Private and public sector employers, including state and local governments, federal agencies, and employment agencies, must abide by the new guidelines unless they can provide evidence that doing so will cause undue hardship.
Female doctors have historically encountered significant barriers to family planning. Years of training cause them to delay having children, often leading to higher rates of infertility, miscarriage, and pregnancy complications than in the general population.
Some specialties, like surgeons, are particularly at risk, with 42% reporting at least one pregnancy loss. Most surgeons work their regular schedules until delivery despite desiring workload reductions, commonly citing unsupportive workplaces as a reason for not seeking accommodations.
Trauma surgeon Qaali Hussein, MD, became pregnant with her first child during her intern year in 2008. She told this news organization that her residency program didn’t even have a maternity policy at the time, and her male supervisor was certain that motherhood would end her surgical career.
She shared how “women usually waited until the end of their training to get pregnant. No one had ever gotten pregnant during the program and returned from maternity leave. I was the first to do so, so there wasn’t a policy or any program support to say, ‘What can we do to help?’ ”
Dr. Hussein used her vacation and sick time, returning to work 4 weeks after delivery. She had five more children, including twins her chief year and another baby during fellowship training in 2014.
Each subsequent pregnancy was met with the same response from program leadership, she recalled. “They’d say, ‘This is it. You may have been able to do the first and second child, but this one will be impossible.’ ”
After the PWFA regulations first became enforceable in June, the EEOC accepted public feedback. The guidelines received nearly 100,000 comments, spurred mainly by the inclusion of abortion care as a qualifying condition for which an employee could receive accommodations. About 54,000 comments called for abortion to be excluded from the final rule, and 40,000 supported keeping the clause.
The EEOC issued the final rule on April 15. It includes abortion care. However, the updated rule “does not require any employee to have — or not to have — an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions,” the unpublished version of the final rule said. It is scheduled to take effect 60 days after its publication in the Federal Register on April 19.
Increasing Support for Doctor-Moms
The PWFA supplements other EEOC protections, such as pregnancy discrimination under Title VII of the Civil Rights Act of 1964 and access to reasonable accommodations under the Americans with Disabilities Act. In addition, it builds upon Department of Labor regulations, like the PUMP Act for breastfeeding employees and the Family and Medical Leave Act, which provides 12 weeks of unpaid, job-protected leave for the arrival of a child or certain medical conditions.
FMLA applies only to employees who have worked full-time for at least 12 months for an employer with 50 or more employees. Meanwhile, the unpaid, job-protected leave under the PWFA has no waiting period, lowers the required number of employees to 15, and permits accommodations for up to 40 weeks.
Employers are encouraged to honor “common and simple” requests, like using a closer parking space or pumping or nursing at work, without requiring a doctor’s note, the rule said.
Efforts to improve family leave policies for physicians and residents have been gaining traction. In 2021, the American Board of Medical Specialties began requiring its member boards with training programs lasting 2 or more years to allow at least 6 weeks off for parental, caregiver, and medical leave. This time can be taken without exhausting vacation or sick leave or requiring an extension in training. Over half of the 24 member boards permit leave beyond 6 weeks, including the American Boards of Allergy and Immunology, Emergency Medicine, Family Medicine, Radiology, and Surgery.
Estefania Oliveros, MD, MSc, cardiologist and assistant professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, told this news organization that the Accreditation Council for Graduate Medical Education also requires that residents and fellows receive 6 weeks of paid leave.
“We add to that vacation time, so it gives them at least 8 weeks,” she said. The school has created spaces for nursing mothers — something neither she nor Dr. Hussein had access to when breastfeeding — and encourages the attendings to be proactive in excusing pregnant fellows for appointments.
This differs significantly from her fellowship training experience 6 years ago at another institution, where she worked without accommodations until the day before her cesarean delivery. Dr. Oliveros had to use all her vacation time for recovery, returning to the program after 4 weeks instead of the recommended 6.
“And that’s the story you hear all the time. Not because people are ill-intended; I just don’t think the system is designed to accommodate women, so we lose a lot of talent that way,” said Dr. Oliveros, whose 2019 survey in the Journal of the American College of Cardiology called for more support and protections for pregnant doctors.
Both doctors believe the PWFA will be beneficial but only if leadership in the field takes up the cause.
“The cultures of these institutions determine whether women feel safe or even confident enough to have children in medical school or residency,” said Dr. Hussein.
A version of this article appeared on Medscape.com.
Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Opportunity Commission (EEOC). The guidelines could prevent women from losing critical career momentum.
The Pregnant Workers Fairness Act (PWFA) aims to help workers balance professional demands with healthy pregnancies. It requires employers to provide reasonable accommodations for a “worker’s known limitations,” including physical or mental conditions associated with “pregnancy, childbirth, or related medical conditions.”
Reasonable accommodations vary but may involve time off to attend healthcare appointments or recover from childbirth, extra breaks during a shift, shorter work hours, or the ability to sit instead of stand. Private and public sector employers, including state and local governments, federal agencies, and employment agencies, must abide by the new guidelines unless they can provide evidence that doing so will cause undue hardship.
Female doctors have historically encountered significant barriers to family planning. Years of training cause them to delay having children, often leading to higher rates of infertility, miscarriage, and pregnancy complications than in the general population.
Some specialties, like surgeons, are particularly at risk, with 42% reporting at least one pregnancy loss. Most surgeons work their regular schedules until delivery despite desiring workload reductions, commonly citing unsupportive workplaces as a reason for not seeking accommodations.
Trauma surgeon Qaali Hussein, MD, became pregnant with her first child during her intern year in 2008. She told this news organization that her residency program didn’t even have a maternity policy at the time, and her male supervisor was certain that motherhood would end her surgical career.
She shared how “women usually waited until the end of their training to get pregnant. No one had ever gotten pregnant during the program and returned from maternity leave. I was the first to do so, so there wasn’t a policy or any program support to say, ‘What can we do to help?’ ”
Dr. Hussein used her vacation and sick time, returning to work 4 weeks after delivery. She had five more children, including twins her chief year and another baby during fellowship training in 2014.
Each subsequent pregnancy was met with the same response from program leadership, she recalled. “They’d say, ‘This is it. You may have been able to do the first and second child, but this one will be impossible.’ ”
After the PWFA regulations first became enforceable in June, the EEOC accepted public feedback. The guidelines received nearly 100,000 comments, spurred mainly by the inclusion of abortion care as a qualifying condition for which an employee could receive accommodations. About 54,000 comments called for abortion to be excluded from the final rule, and 40,000 supported keeping the clause.
The EEOC issued the final rule on April 15. It includes abortion care. However, the updated rule “does not require any employee to have — or not to have — an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions,” the unpublished version of the final rule said. It is scheduled to take effect 60 days after its publication in the Federal Register on April 19.
Increasing Support for Doctor-Moms
The PWFA supplements other EEOC protections, such as pregnancy discrimination under Title VII of the Civil Rights Act of 1964 and access to reasonable accommodations under the Americans with Disabilities Act. In addition, it builds upon Department of Labor regulations, like the PUMP Act for breastfeeding employees and the Family and Medical Leave Act, which provides 12 weeks of unpaid, job-protected leave for the arrival of a child or certain medical conditions.
FMLA applies only to employees who have worked full-time for at least 12 months for an employer with 50 or more employees. Meanwhile, the unpaid, job-protected leave under the PWFA has no waiting period, lowers the required number of employees to 15, and permits accommodations for up to 40 weeks.
Employers are encouraged to honor “common and simple” requests, like using a closer parking space or pumping or nursing at work, without requiring a doctor’s note, the rule said.
Efforts to improve family leave policies for physicians and residents have been gaining traction. In 2021, the American Board of Medical Specialties began requiring its member boards with training programs lasting 2 or more years to allow at least 6 weeks off for parental, caregiver, and medical leave. This time can be taken without exhausting vacation or sick leave or requiring an extension in training. Over half of the 24 member boards permit leave beyond 6 weeks, including the American Boards of Allergy and Immunology, Emergency Medicine, Family Medicine, Radiology, and Surgery.
Estefania Oliveros, MD, MSc, cardiologist and assistant professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, told this news organization that the Accreditation Council for Graduate Medical Education also requires that residents and fellows receive 6 weeks of paid leave.
“We add to that vacation time, so it gives them at least 8 weeks,” she said. The school has created spaces for nursing mothers — something neither she nor Dr. Hussein had access to when breastfeeding — and encourages the attendings to be proactive in excusing pregnant fellows for appointments.
This differs significantly from her fellowship training experience 6 years ago at another institution, where she worked without accommodations until the day before her cesarean delivery. Dr. Oliveros had to use all her vacation time for recovery, returning to the program after 4 weeks instead of the recommended 6.
“And that’s the story you hear all the time. Not because people are ill-intended; I just don’t think the system is designed to accommodate women, so we lose a lot of talent that way,” said Dr. Oliveros, whose 2019 survey in the Journal of the American College of Cardiology called for more support and protections for pregnant doctors.
Both doctors believe the PWFA will be beneficial but only if leadership in the field takes up the cause.
“The cultures of these institutions determine whether women feel safe or even confident enough to have children in medical school or residency,” said Dr. Hussein.
A version of this article appeared on Medscape.com.
<!--$RCSfile: InCopy_agile.xsl,v $ $Revision: 1.35 $-->
<!--$RCSfile: drupal.xsl,v $ $Revision: 1.7 $-->
<root generator="drupal.xsl" gversion="1.7"> <header> <fileName>167809</fileName> <TBEID>0C04FBCA.SIG</TBEID> <TBUniqueIdentifier>MD_0C04FBCA</TBUniqueIdentifier> <newsOrJournal>News</newsOrJournal> <publisherName>Frontline Medical Communications</publisherName> <storyname/> <articleType>2</articleType> <TBLocation>QC Done-All Pubs</TBLocation> <QCDate>20240422T165833</QCDate> <firstPublished>20240422T165844</firstPublished> <LastPublished>20240422T165844</LastPublished> <pubStatus qcode="stat:"/> <embargoDate/> <killDate/> <CMSDate>20240422T165844</CMSDate> <articleSource/> <facebookInfo/> <meetingNumber/> <byline>Steph Weber</byline> <bylineText>STEPH WEBER</bylineText> <bylineFull>STEPH WEBER</bylineFull> <bylineTitleText/> <USOrGlobal/> <wireDocType/> <newsDocType>News</newsDocType> <journalDocType/> <linkLabel/> <pageRange/> <citation/> <quizID/> <indexIssueDate/> <itemClass qcode="ninat:text"/> <provider qcode="provider:imng"> <name>IMNG Medical Media</name> <rightsInfo> <copyrightHolder> <name>Frontline Medical News</name> </copyrightHolder> <copyrightNotice>Copyright (c) 2015 Frontline Medical News, a Frontline Medical Communications Inc. company. All rights reserved. This material may not be published, broadcast, copied, or otherwise reproduced or distributed without the prior written permission of Frontline Medical Communications Inc.</copyrightNotice> </rightsInfo> </provider> <abstract/> <metaDescription>Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Oppor</metaDescription> <articlePDF/> <teaserImage/> <teaser>Newly updated guidelines for the federal Pregnant Workers Fairness Act could help physicians better balance career and family.</teaser> <title>New Federal Rule Delivers Workplace Support, Time Off for Pregnant Docs</title> <deck/> <disclaimer/> <AuthorList/> <articleURL/> <doi/> <pubMedID/> <publishXMLStatus/> <publishXMLVersion>1</publishXMLVersion> <useEISSN>0</useEISSN> <urgency/> <pubPubdateYear/> <pubPubdateMonth/> <pubPubdateDay/> <pubVolume/> <pubNumber/> <wireChannels/> <primaryCMSID/> <CMSIDs/> <keywords/> <seeAlsos/> <publications_g> <publicationData> <publicationCode>im</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>rn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>pn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>oncr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>ob</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>nr</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle>Neurology Reviews</journalTitle> <journalFullTitle>Neurology Reviews</journalFullTitle> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>mdsurg</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement>2018 Frontline Medical Communications Inc.,</copyrightStatement> </publicationData> <publicationData> <publicationCode>mdemed</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement/> </publicationData> <publicationData> <publicationCode>mdid</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>hemn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>fp</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>skin</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>cpn</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>endo</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>chph</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>card</publicationCode> <pubIssueName/> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> </publicationData> <publicationData> <publicationCode>GIHOLD</publicationCode> <pubIssueName>January 2014</pubIssueName> <pubArticleType/> <pubTopics/> <pubCategories/> <pubSections/> <journalTitle/> <journalFullTitle/> <copyrightStatement/> </publicationData> </publications_g> <publications> <term canonical="true">21</term> <term>26</term> <term>25</term> <term>31</term> <term>23</term> <term>22</term> <term>52226</term> <term>58877</term> <term>51892</term> <term>18</term> <term>15</term> <term>13</term> <term>9</term> <term>34</term> <term>6</term> <term>5</term> </publications> <sections> <term canonical="true">27980</term> <term>39313</term> </sections> <topics> <term>322</term> <term canonical="true">38029</term> <term>50194</term> <term>278</term> </topics> <links/> </header> <itemSet> <newsItem> <itemMeta> <itemRole>Main</itemRole> <itemClass>text</itemClass> <title>New Federal Rule Delivers Workplace Support, Time Off for Pregnant Docs</title> <deck/> </itemMeta> <itemContent> <p>Pregnant physicians may receive more workplace accommodations and protection against discrimination thanks to an updated rule from the US Equal Employment Opportunity Commission (EEOC). The guidelines could prevent women from losing critical career momentum. </p> <p>The <span class="Hyperlink"><a href="https://www.eeoc.gov/newsroom/eeoc-issues-final-regulation-pregnant-workers-fairness-act">Pregnant Workers Fairness Act (PWFA)</a></span> aims to help workers balance professional demands with healthy pregnancies. It requires employers to provide reasonable accommodations for a “worker’s known limitations,” including physical or <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/restricted-abortion-access-tied-mental-health-harm-2024a10001u9">mental conditions</a></span> associated with “pregnancy, childbirth, or related medical conditions.”<br/><br/>Reasonable accommodations vary but may involve time off to attend healthcare appointments or recover from childbirth, extra breaks during a shift, shorter work hours, or the ability to sit instead of stand. Private and public sector employers, including state and local governments, federal agencies, and employment agencies, must abide by the new guidelines unless they can provide evidence that doing so will cause undue hardship. <br/><br/>Female doctors have historically encountered <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/987608">significant barriers</a></span> to family planning. Years of training cause them to delay having children, often leading to higher rates of <span class="Hyperlink">infertility</span>, <span class="Hyperlink">miscarriage</span>, and pregnancy complications than in the general population. <br/><br/>Some specialties, like surgeons, are particularly <span class="Hyperlink"><a href="https://www.sciencedirect.com/science/article/abs/pii/S0022480423000987">at risk</a></span>, with 42% reporting at least one <span class="Hyperlink"><a href="https://reference.medscape.com/article/266317-overview">pregnancy loss</a></span>. Most surgeons work their regular schedules until delivery despite desiring workload reductions, commonly citing unsupportive workplaces as a reason for not seeking accommodations. <br/><br/>Trauma surgeon Qaali Hussein, MD, became pregnant with her first child during her intern year in 2008. She told this news organization that her residency program didn’t even have a maternity policy at the time, and her male supervisor was certain that motherhood would end her surgical career. <br/><br/>She shared how “women usually waited until the end of their training to get pregnant. No one had ever gotten pregnant during the program and returned from maternity leave. I was the first to do so, so there wasn’t a policy or any program support to say, ‘What can we do to help?’ ”<br/><br/>Dr. Hussein used her vacation and sick time, returning to work 4 weeks after delivery. She had five more children, including twins her chief year and another baby during fellowship training in 2014. <br/><br/>Each subsequent pregnancy was met with the same response from program leadership, she recalled. “They’d say, ‘This is it. You may have been able to do the first and second child, but this one will be impossible.’ ”<br/><br/>After the PWFA regulations first became enforceable in June, the EEOC accepted public feedback. The guidelines received <span class="Hyperlink"><a href="https://www.regulations.gov/document/EEOC-2023-0004-0001">nearly 100,000 comments</a></span>, spurred mainly by the inclusion of abortion care as a qualifying condition for which an employee could receive accommodations. About 54,000 comments called for abortion to be excluded from the final rule, and 40,000 supported keeping the clause. <br/><br/>The EEOC issued the final rule on April 15. It includes abortion care. However, the updated rule “does not require any employee to have — or not to have — an abortion, does not require taxpayers to pay for any abortions, and does not compel health care providers to provide any abortions,” the <span class="Hyperlink"><a href="https://www.federalregister.gov/public-inspection/2024-07527/implementation-of-the-pregnant-workers-fairness-act">unpublished version</a></span> of the final rule said. It is scheduled to take effect 60 days after its publication in the Federal Register on April 19.<br/><br/></p> <h2>Increasing Support for Doctor-Moms</h2> <p>The PWFA supplements other EEOC protections, such as pregnancy discrimination under Title VII of the Civil Rights Act of 1964 and access to reasonable accommodations under the Americans with Disabilities Act. In addition, it builds upon Department of Labor regulations, like the PUMP Act for <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/979276">breastfeeding employees</a></span> and the Family and Medical Leave Act, which provides 12 weeks of unpaid, job-protected leave for the arrival of a child or certain medical conditions.</p> <p>FMLA applies only to employees who have worked full-time for at least 12 months for an employer with 50 or more employees. Meanwhile, the unpaid, job-protected leave under the PWFA has no waiting period, lowers the required number of employees to 15, and permits accommodations for up to 40 weeks. <br/><br/>Employers are encouraged to honor “common and simple” requests, like using a closer parking space or pumping or nursing at work, without requiring a doctor’s note, the rule said. <br/><br/>Efforts to improve family leave policies for physicians and residents have been gaining traction. In 2021, the American Board of Medical Specialties began <span class="Hyperlink"><a href="https://www.abms.org/newsroom/abms-member-boards-leave-policies-help-residents-care-for-their-own-families/">requiring its member boards</a></span> with training programs lasting 2 or more years to allow at least 6 weeks off for parental, caregiver, and medical leave. This time can be taken without exhausting vacation or sick leave or requiring an extension in training. Over half of the 24 member boards permit leave beyond 6 weeks, including the American Boards of Allergy and Immunology, Emergency Medicine, Family Medicine, Radiology, and Surgery. <br/><br/>Estefania Oliveros, MD, MSc, cardiologist and assistant professor at the Lewis Katz School of Medicine at Temple University, Philadelphia, told this news organization that the Accreditation Council for Graduate Medical Education also requires that residents and fellows receive <span class="Hyperlink">6 weeks of paid leave</span>. <br/><br/>“We add to that vacation time, so it gives them at least 8 weeks,” she said. The school has created spaces for nursing mothers — something neither she nor Dr. Hussein had access to when breastfeeding — and encourages the attendings to be proactive in excusing pregnant fellows for appointments. <br/><br/>This differs significantly from her fellowship training experience 6 years ago at another institution, where she worked without accommodations until the day before her <span class="Hyperlink">cesarean delivery</span>. Dr. Oliveros had to use all her vacation time for recovery, returning to the program after 4 weeks instead of the recommended 6. <br/><br/>“And that’s the story you hear all the time. Not because people are ill-intended; I just don’t think the system is designed to accommodate women, so we lose a lot of talent that way,” said Dr. Oliveros, whose 2019 <span class="Hyperlink"><a href="https://www.jacc.org/doi/10.1016/j.jaccas.2019.05.028">survey</a></span> in the <em>Journal of the American College of Cardiology</em> called for more support and protections for pregnant doctors. <br/><br/>Both doctors believe the PWFA will be beneficial but only if leadership in the field takes up the cause. <br/><br/>“The cultures of these institutions determine whether women feel safe or even confident enough to have children in medical school or residency,” said Dr. Hussein. <br/><br/></p> <p> <em>A version of this article appeared on <span class="Hyperlink"><a href="https://www.medscape.com/viewarticle/new-federal-rule-delivers-workplace-support-time-pregnant-2024a10007k1">Medscape.com</a></span>.</em> </p> </itemContent> </newsItem> <newsItem> <itemMeta> <itemRole>teaser</itemRole> <itemClass>text</itemClass> <title/> <deck/> </itemMeta> <itemContent> </itemContent> </newsItem> </itemSet></root>
